The portable MicroMaxx ultrasound system from Sonosite can be easily hand carried to wherever needed.
A clot that forms in the deep vein in either the leg or pelvic region is known as a deep vein thrombosis (DVT), an increasingly common venous disease, which according to the American Health Association is diagnosed in one out of every 1,000 Americans each year. While DVTs themselves are not life-threatening, if a clot breaks free it can travel, raising the patient’s risk for heart attack, stroke or pulmonary embolism.
Awareness of the disease heightened earlier this year when Vice President Dick Cheney suffered a DVT after a nine-day, 25,000-mile overseas trip. Up until that time many Americans were unfamiliar with the condition and the fact that something as seemingly innocuous as prolonged sitting can be the cause. According to the National Institutes for Health, even 90 minutes of uninterrupted sitting can raise an individual’s risk of developing a clot. Other risk factors include obesity, family history, surgery, hypercoagulability and the use of certain medications.
Unlocking the keys to detection
The link between DVT and potentially fatal incidences underscores the importance of detection. Unfortunately, because DVTs often mimic other conditions, or worse, are asymptomatic, they can be difficult to diagnose.
A D-dimer assay is a rapid initial test for DVT that detects elevated fibrinogen — a protein that affects clotting — levels in the blood. While some practitioners question the value of D-dimer studies, the test’s positive result may indicate the presence of a clot or pulmonary embolism, which an imaging exam can then conclusively confirm or deny. Ultrasound imaging, which uses Doppler to determine the direction and speed of blood flow, is currently the most commonly used imaging method for DVT detection. It is a quick, real-time test that requires no radiation and is considered the first line diagnostic test for DVT in the leg.
David Vanderpool, M.D., who specializes in the management of venous disease, relies on Sonosite’s MicroMaxx hand-carried ultrasound system for all his venous imaging needs. The system offers a full complement of quick-change, lightweight transducers for all venous/vein care applications including DVT, vein mapping, venous reflux studies and venous ablation guidance.
“Most vascular surgeons are pretty well trained in arterial ultrasound, but less so in venous ultrasound. Regardless of training, the MicroMaxx is user friendly and outstanding for vein work,” Dr. Vanderpool said.
The MicroMaxx can also send images wirelessly to a hospitals’ DICOM server.
“One of the most convenient features of the MicroMaxx system is that it’s a digital system,” Dr. Vanderpool said. With a wireless interface, images can be saved from the MicroMaxx directly to the computer, and authorized personnel can access them as soon as they are transferred, he explained.
One drawback of ultrasound is that it is less able than other techniques to visualize veins in the pelvis. In addition, accurate results are dependent on the skills of the technologist administering the test. However, experts agree that when performed correctly, an ultrasound exam is an excellent tool for detecting proximal lower extremity DVT.
Magnetic resonance imaging (MRI) is able to detect thromboses not only in the abdomen and extremities, but also in the deep veins of the pelvis. In fact, estimates of MR venography’s sensitivity and specificity for detecting lower extremity DVT are as high as 100 percent.1
“The question then becomes: How much is that additional sensitivity or specificity worth?“ said Jeffrey Maki, M.D., Ph.D., a radiologist at Puget Sound VA Hospital and University of Washington Medical Center, Seattle. “MR is a more expensive, more complicated and lengthier procedure compared to ultrasound,” said Dr. Maki. In my experience, he explains, MR is a special-use tool used in situations where a pelvic DVT is suspected.
Cardiovascular radiologist Steven Wolff, M.D., Ph.D., director of Advanced Cardiovascular Imaging, New York City, and assistant professor at Columbia University, however, believes “MRI is a great tool for venous imaging.“
“MR can pick up clots better than ultrasound especially if the clots are below the knee or in the pelvis. I would recommend that everyone with a high clinical suspicion for DVT and a negative ultrasound get a MRI,” he said.
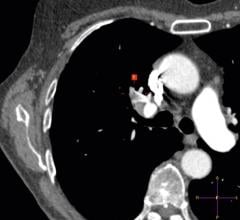
That may be good advice because when an ultrasound is negative for DVT, often further studies are not ordered. As a result, “there are probably occult DVTs in the pelvis that are not being recognized,” said Dr. Maki. He cites a paper he co-wrote with neurologist Steve Cramer, M.D., in which they explore MR venography in the pelvis on patients with cryptogenic stroke. The authors theorize that for a certain population — those who have a hole between the left and right heart — a pelvic DVT can embolize in the left heart and travel to the brain, causing a stroke.
Dr. Maki also discusses of an exciting new technology already approved in Europe and Asia that may propel MR into the mainstream for DVT detection in the leg or pelvis. Vasovist is a blood pool contrast agent for MRI that when injected stays in the vascular space with a half-life of about one to two hours and produces beautiful images, says Dr. Maki. Based on preliminary studies, an exam of the pelvis and extremities can be performed in as little as five to 10 minutes and is not reliant on time-of-flight or phased-contrast techniques. The vessels appear bright because they are filled with contrast, and a thrombus shows up as a black linear defect.
“Vasovist will be a very robust, more complete examination,” explained Dr. Maki. “We’ll be able to scan multiple areas of interest with one injection of contrast, making DVT mapping of multiple anatomical segments possible.”
The imaging debate aside, one thing is certain — early detection is the key to short-circuiting DVT’s potentially serious consequences and possibly saving a patient’s life.
Reference:
Diagnosis of Lower Extremity Deep Vein Thrombosis,
www.massgeneralimaging.org/newsletter/may_2005



 November 21, 2022
November 21, 2022