February 10, 2016 — CeloNova BioSciences Inc. announced this week that the first patient has been enrolled in its COBRA REDUCE trial. The COBRA REDUCE trial recently received conditional U.S. Food and Drug Administration (FDA) approval and will study the Cobra PzF nanocoated coronary stent (NCS) system in patients at high risk of bleeding.
The first stent in the trial was implanted at the Northshore University Hospital, New York by Loukas Boutis, M.D. Eventually, 844 patients will be enrolled in the clinical trial both in the United States and Europe.
Rajiv Jauhar, M.D., chief of cardiology and director cardiac catheterization labs at the Northshore University Hospital in New York, said, “We are excited to be part of this second, very important, trial with the COBRA PzF stent. We were the highest enrolling center in the initial PzF SHIELD trial with the COBRA PzF stent and hope to repeat our achievement.”
About one in five patients are at high risk of bleeding after stenting. Complications from bleeding after percutaneous coronary intervention (PCI) occur more frequently than myocardial infarctions and have a greater impact on mortality. The trial will evaluate if the Cobra PzF stent, with its novel Polyzene-F nanocoating and advanced thin-strut design, can help reduce bleeding as compared to drug eluting stents (DES), by shortening the duration of dual antiplatelet therapy (DAPT) to 14 days in patients treated with oral anticoagulation and undergoing PCI.
“For patients with high risk of bleeding such as those on triple therapy, the optimal duration of DAPT and type of stent are important questions,” said Adnan Kastrati, M.D., professor of medicine at Deutsches Herzzentrum, München, Germany and the principal investigator of the trial.
”If the COBRA PzF stent, with its novel nanocoating, is able to reduce the duration of DAPT to only two weeks and to reduce bleeding, while maintaining parity with DES in thrombosis and restenosis, it could be a very compelling new treatment option.”
The COBRA REDUCE trial is the second major interventional cardiology trial for CeloNova and follows a successful early enrollment completion of the PzF SHIELD investigational device exemption (IDE) study last year. Positive results from the PzF SHIELD study will allow the company to complete its premarket application to the FDA for the Cobra PzF stent.
These trials are part of a comprehensive clinical program studying over 2,000 patients worldwide. Previous peer-reviewed studies with over 700 patients implanted with the prior generation stent coated with the Polyzene-F nanocoating demonstrated low target lesion revascularization (TLR) and no stent thrombosis.
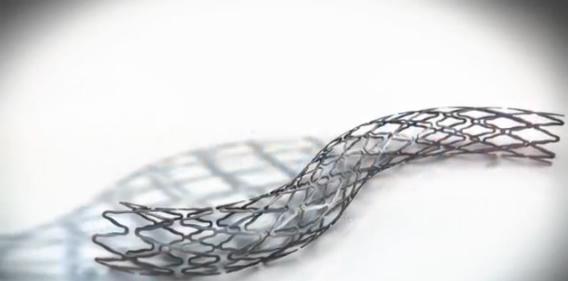
The Cobra PzF stent has thin struts made of cobalt chromium super alloy and is coated with an advanced Polyzene-F nanocoating, which may reduce fibrinogen and platelet adhesion as shown in preclinical studies. Furthermore, the stent platform is designed to minimize vessel wall injury and lower inflammation as demonstrated in preclinical studies.
The Cobra PzF coronary stent system is an investigational device in the United States. It received CE Mark approval in 2012 and launched in Europe and the Middle East in 2013.
For more information: www.celonova.com


 November 14, 2025
November 14, 2025 









