April 18, 2019 — The U.S. Food and Drug Administration published a draft guidance titled, “Technical Considerations for Non-Clinical Assessment of Medical Devices Containing Nitinol,” which includes proposed recommendations on what manufacturers should include in their premarket submission of a device containing nitinol, an alloy of nickel and titanium. The recommendations include testing to evaluate susceptibility to corrosion, biocompatibility and performance under certain conditions of stress/strain or temperature, and labeling — including language about the risk of potential allergic reactions to the metals — and information on how the device is manufactured and other factors that could affect the breakdown of the material in the body.
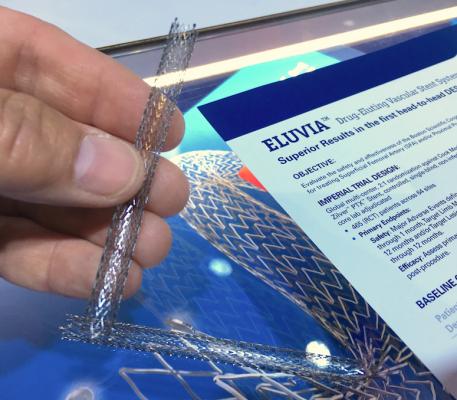
Nitinol is a commonly used material in the medical device industry, including in orthodontic archwires, cardiovascular guidewires and stents, surgical instruments, orthopedic fracture fixation, transcatheter heart valves and the permanent birth control implant Essure. The FDA had previously issued guidance titled, “Select Updates for Non-Clinical Engineering Tests and Recommended Labeling for Intravascular Stents and Associated Delivery Systems,” which provided recommendations on corrosion and nickel-ion release testing for certain cardiac devices that may contain nitinol. Because that guidance was specific only to intravascular stents and delivery systems, and with the expansion of nitinol into other product areas, the agency is issuing this cross-cutting draft guidance document to explore broadening its recommendations to any device that contains nitinol.
Earlier this year, the FDA announced a broad effort to engage the public, scientists and industry stakeholders to gather information about medical device materials. The goal of this effort is to ensure the current state of the science is reflected in agency decision-making, to identify any critical gaps in the existing science that need to be addressed, and to determine what approaches should be considered to further understanding of the materials and improve the safety of devices for patients.
Today’s draft guidance, once finalized, will provide additional clarity to device manufacturers regarding information the FDA intends to consider as part of the premarket review process with the use of nitinol in devices.
“The materials used in devices are important, both to the function of the device and to the safety of the device because of how the human body may respond to the materials used. That’s why we’ve committed to taking steps to advance the science underlying the effects of specific materials, including nitinol, to inform our evaluation of devices and support the development screening tools to assess potential health risks to individual patients,” said Jeff Shuren, M.D., J.D., director of the FDA’s Center for Devices and Radiological Health. “Nitinol has unique properties that have led to an increase in its use in devices – particularly for orthopedic fracture fixation, cardiovascular stents, guidewires and other devices used in minimally-invasive medical procedures. Devices made with nitinol provide many important benefits to patients, but we need to be able to assess whether, among other things, there are any health risks when the material comes into contact with various parts of the body for extended periods of time. To ensure that the benefits patients receive from these devices outweigh any risks resulting from their use, the FDA needs to receive the right information as part of the premarket review process. To that end, today we are providing manufacturers with a proposal for the types of information they should include in their premarket submission of a device containing nitinol, including testing, labeling, and information on how the device is manufactured and other factors that could affect the breakdown of the material in the body.”
For more information: www.fda.gov


 November 14, 2025
November 14, 2025 









