July 22, 2015 — Heart failure patients had a significantly lower chance of being readmitted within 30 days of discharge when treated with a cardiac resynchronization therapy device (CRT) equipped with an algorithm to automatically deliver and adjust therapy, according to a recent study in JACC: Heart Failure. The study compared these patients to those receiving the standard CRT optimized with echocardiography.
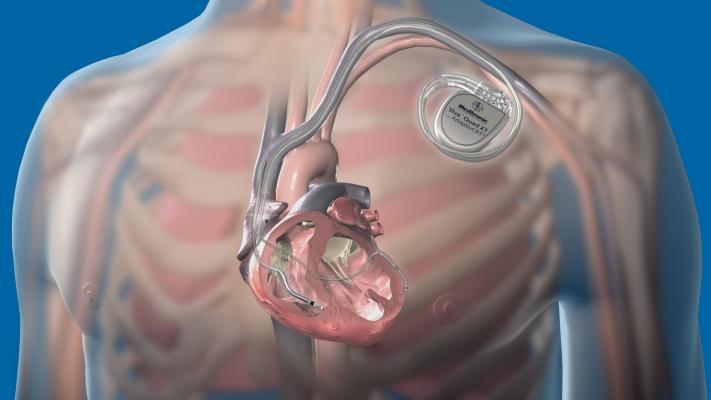
A CRT device is a defibrillator that sends electrical impulses to the heart to help the chambers beat in synchronization and improves the heart's pumping function. It is an established treatment for patients with heart failure, and while it has been proven to provide many benefits, including an improved quality of life and reduced risk of death, not all patients respond to CRT.
In this study, researchers analyzed data from the Adaptive CRT trial to determine rates of hospital readmissions for heart failure patients with a CRT device. For heart failure hospitalizations the 30-day readmission rate was 19.1 percent in patients with the AdaptivCRT algorithm and 35.7 percent in patients with echo. For all-cause hospitalization, the 30-day readmission rate was 14.8 percent with the algorithm compared to 24.8 percent with echo. The risk reduction for readmission was also signficantly reduced beyond 30 days.
Heart failure was one of the first hospitalization types to be identified under the Hospital Readmissions Reduction Program, which reduces Medicare inpatient payments when a patient is readmitted to the hospital within 30 days of discharge for certain conditions. According to the study, the CRT algorithm showed a significant reduction in 30-day readmission rates, making it a potential safe and effective strategy to reduce readmissions and overall health care costs.
For more information: www.acc.org


 February 03, 2026
February 03, 2026 









