October 11, 2017 — An analysis of more than 1,000 minimally invasive aortic valve replacements and more than 400 additional associated procedures over a five-and-a-half year period showed low stroke rates and high survival rates in all age groups within 30 days of surgery. All procedures were performed by Joseph Lamelas, M.D., professor and associate chief of cardiac surgery in the division of cardiothoracic surgery at Baylor College of Medicine. His report appears in the Journal of Thoracic and Cardiovascular Surgery.
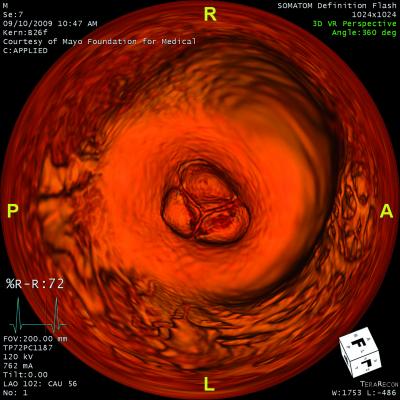
Aortic valve replacements are performed when treating aortic valve stenosis or aortic valve regurgitation. Aortic valve stenosis occurs when the aortic valve opening is narrowing and restricts the blood flow from the left ventricle to the aorta. This makes the heart work harder to pump blood to the body. Aortic valve regurgitation takes place when there is a leakage of blood through the aortic valve into the left ventricle.
Lamelas performs a minimally invasive procedure to replace the aortic valve. The procedure requires only a two-inch incision between the ribs rather than opening the breast bone. This results in a shorter stay in the hospital and a faster recovery time.
To document the results of this particular approach, Lamelas assessed more than 1,000 of his aortic valve replacement procedures over a five-and-a-half year period. He also assessed more than 400 additional concomitant procedures, meaning the patient had an aortic valve procedure with another procedure such as mitral valve repair or ascending aorta replacement. The procedures were performed when Lamelas was with Mount Sinai Heart Institute in Miami Beach, Fla., between January 2009 and July 2015.
Lamelas and colleagues compared patients less than 80 years old to those over 80 years old.
They found the mortality rate in patients who only had the aortic valve replacement was 1.3 percent and 3.2 percent in the group that had a concomitant procedure. The risk of stroke was 0.8 percent and 1.1 percent, respectively, in both age groups.
“We found that the risk for mortality and stroke was a little bit higher for older patients, but not statistically significant compared to the younger patients,” said Lamelas.
In addition, they found low rates of complication in all age groups, a significantly reduced length of stay in the hospital, low postoperative complication rates and a low postoperative length of stay. In the concomitant group, results also were similar.
“These results further demonstrate that there is no need to do a full sternotomy if we have this procedure available,” said Lamelas, who is a pioneer in the field of minimally invasive heart surgery and has developed facilitating instruments for the procedure.
Lamelas receives honoraria from Medtronic, St. Jude and On-Q and has ownership interest in Miami Instruments.
For more information: www.jtcvsonline.org


 January 15, 2026
January 15, 2026 









