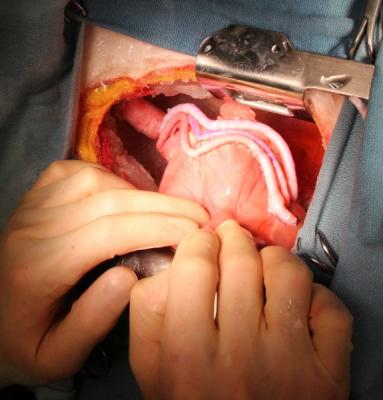
Multiple repetitions of bypass grafts on a heart, using the Ramphal simulator. Courtesy of the University of Washington in Seattle.
August 25, 2016 — Simulation training for surgery residents builds confidence and could have a life-saving impact on patients undergoing cardiac surgery, according to two studies published online in The Annals of Thoracic Surgery.
“Simulation training should create better surgeons who are trained much more efficiently,” said Richard H. Feins, M.D., from the University of North Carolina at Chapel Hill, who led one of the studies. “This type of learning allows surgery residents to develop their knowledge, skills and confidence before going into the operating room, thus protecting patients from unnecessary risks.”
Feins, along with Nahush A. Mokadam, M.D., from the University of Washington in Seattle, and James I. Fann, M.D., from Stanford University in California, were among leaders from eight major cardiothoracic surgery residency programs in the United States who formed the Cardiac Surgery Simulation Consortium.
In what is believed to be the largest, most comprehensive study of simulation-based cardiac surgery training ever conducted, the Consortium developed a rigorous, 39-session curriculum that included simulation training modules for three commonly performed cardiac surgery procedures (cardiopulmonary bypass, coronary artery bypass grafting and aortic valve replacement) and three adverse events (unexpected and undesirable experiences, such as a sudden deterioration in heart function).
“The first three modules laid out the basics of cardiac surgery,” said Mokadam. “We had 27 residents who were taught in a deliberate, detailed, progressive manner that ensured they understood the basics. Over the course of several weeks, the residents went from novices to truly being experts in doing routine procedures such as aortic valve replacement.” The second half of the curriculum delved into adverse events. Residents were instructed in a non-threatening classroom environment on how to address catastrophes during surgery, and then practiced their protocols in a fully immersive simulated environment.
The simulation technology ranged from low-fidelity plastic models to real tissue and pig hearts that realistically duplicated actual patients undergoing surgery. Repetition, practice, coaching and review were incorporated into each module and resulted in a significant improvement in surgical skills, communication and decision-making. The study showed that cardiothoracic surgery residents improved in all surgical skills that were evaluated, with perfect or near perfect performance after about 110 hours of total simulation training per resident.
Traditionally, surgery residents are taught to perform surgery via the apprenticeship model, which depends on learning almost exclusively in the operating room. According to Feins, the modern operating room is too fast-paced and has too many competing priorities to be the only place to train residents. A simulation-based curriculum can enhance and facilitate training by circumventing the limitations of the operating room, thus providing a model to complement the traditional apprentice learning in medicine.
“In the simulation environment, the essentials of producing masters — deliberate practice and component task training — can be employed,” said Feins. “One would never expect to produce an outstanding basketball team if the players could only develop their skills during a game. But that is essentially what the apprentice model in surgery does. We have shown there is a better way.”
Unlike the operating room, the simulated surgery environment allows learning and re-learning skills as often as required to correct mistakes. This provides the opportunity for residents to fine-tune skills and gain confidence, in an effort to optimize clinical outcomes. The per-repetition analyses from the study showed a clear relationship between repetition of a task and improvement in performance.
“Simulation-based training in adverse events could well prove life-saving,” explained Feins. “This training has the ability to decrease the number of adverse outcomes that occur and to minimize the ramifications of those events. This should result in better outcomes for patients, as well as lower costs and improved efficiency.”
Fann agreed. “We have created a curriculum that allows crisis management training to be conducted during cardiac surgery residency. Until this study, we have not had well-defined steps for simulation-based crisis management of important rare events. This approach leads directly to improved patient safety.”
A companion study, also published online in The Annals, analyzed the experiences of residents and faculty members who participated in the simulation training.
The analysis found that, after completing simulation training, the vast majority of residents (85 percent) and the entire faculty (100 percent) reported feeling more comfortable and confident with the resident skillset and performance in the operating room. The experience also helped residents and faculty develop an improved rapport and confidence in each other.
“The rapport I had with the residents was exponentially improved,” said Mokadam. “I had practiced with the residents in the simulation lab and they had proved to me time and again that they knew the steps and that they understood the principles of the operation. So when we were in the operating room, my confidence level in those residents was extremely high because they had already proved to me that they could do it.”
At the completion of the study, the curriculum was reworked into 29 sessions, rather than 39 sessions. The revised curriculum is now available via the Thoracic Surgery Directors Association, which, along with other organizations, provides leadership in cardiothoracic surgery residency education in the United States. In addition, the Consortium trains faculty members at other residency programs on how to use the curriculum.
“The simulation-based training curriculum will continue to evolve and expand,” said Feins. “This model for training is also being adopted for training in other parts of cardiothoracic surgery such as robotic lobectomy. We hope that it will be an integral part of every resident’s experience in the not so distant future.”
For more information: www.annalsthoracicsurgery.org



 February 06, 2026
February 06, 2026 









