Photo: Penumbra
Oct. 27, 2025 – Penumbra, Inc. has announced the results of the STORM-PE randomized controlled trial (RCT), which found that the use of mechanical thrombectomy, specifically computer assisted vacuum thrombectomy (CAVT), with anticoagulation achieved superior reduction in right heart strain compared to anticoagulation therapy alone in patients with acute intermediate-high risk pulmonary embolism (PE). The data was presented at a late-breaking session during the 37th Annual Transcatheter Cardiovascular Therapeutics (TCT) Conference in San Francisco.
“These findings mark a pivotal step in advancing care for PE, providing the strongest evidence to date that advanced therapy with CAVT can safely improve recovery of the right heart better than conventional anticoagulation therapy,” said Robert Lookstein, MD, MSc; co-global principal investigator of the STORM-PE RCT and professor of radiology and surgery at Icahn School of Medicine at Mount Sinai. “STORM-PE supports the role of CAVT as a more effective therapeutic option for intermediate-high risk patients and will evolve the paradigm of care by delivering rapid relief with a comparable safety profile to anticoagulation alone.”
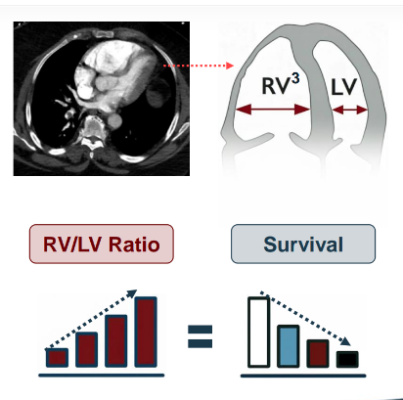
The trial enrolled 100 patients across 22 international sites. Patients treated with CAVT demonstrated a greater reduction in right-to-left ventricular (RV/LV) diameter ratio within 48 hours (mean reduction 0.52 vs. 0.24; P<0.001) and nearly 80% of patients had positive treatment effect with CAVT which was significantly greater than the patients who received anticoagulation (78.3% vs. 51.9%; P =0.011), reflecting rapid hemodynamic recovery.
“What’s particularly compelling is that a significantly greater portion of patients treated with CAVT achieved normalization of RV/LV ratio within 48 hours — a critical indicator of right heart recovery — without an increase in complications,” said Rachel Rosovsky, MD, MPH, co-global principal investigator of STORM-PE RCT and hematologist at the Massachusetts General Hospital. “These findings represent a meaningful advancement in how we approach early intervention and we are eager to see how the changes in RV/LV ratio correlate with other clinical and functional outcomes.”
The rate of major adverse events (MAE) within 7 days — including a composite of PE-related mortality, recurrent PE, clinical deterioration requiring rescue therapy, and major bleeding — was comparable between groups (4.3% [2/47] with CAVT vs. 7.5% [4/53] with anticoagulation alone).
“For the first time, we have prospective, level 1 evidence demonstrating that CAVT, with anticoagulation is superior to anticoagulation alone,” said James F. Benenati, MD, FSIR, chief medical officer at Penumbra. “Combined with Penumbra’s strong prospective data from STRIKE-PE, this randomized evidence from the STORM-PE trial will play a critical role in advancing PE care and supporting the inclusion of CAVT in future treatment guidelines.
”In the U.S., an estimated 900,000 cases of symptomatic venous thromboembolism, which includes PE, occur annuallyi . PE can be life-threatening with 10-30 percent of individuals dying within one month of diagnosis, representing the third leading cause of cardiovascular death after heart attack and strokeii,ii, iii. Penumbra’s Lightning Flash portfolio is the most advanced mechanical thrombectomy system on the market to address venous and pulmonary thrombus. It features Penumbra’s Lightning CAVT technology with the latest dual clot detection algorithms, using both pressure and flow-based processes to detect blood clot and blood flow. The portfolio is designed to help remove blood clots with speed, safety and simplicity, allowing physicians to better navigate the body’s complex anatomy and deliver high power aspiration for clot removal.
Learn more about STORM-PE at www.penumbrainc.com/storm-pe-trial.
Additional results from the STORM-PE trial will be presented at the upcoming VEINS (Venous Endovascular Interventional Strategies) and VIVA (Vascular InterVentional Advances) Conference, taking place in Novembe in Las Vegas, NV.
i “Learn about Pulmonary Embolism,” American Lung Association. Accessed on Oct. 7, 2025. https://www.lung.org/lung-health-diseases/lung-disease-lookup/pulmonary-embolism/learn-about-pulmonary-embolism
ii “Pulmonary Embolism: A Clinical Approach, ” American College of Cardiology. Accessed on Oct. 9, 2025. www.acc.org/Latest-in-Cardiology/Articles/2025/02/01/42/Cover-Story-Pulmonary-Embolism
iii “Learn About Pulmonary Embolism.” American Lung Association. Accessed on Oct. 10, 2025. www.lung.org/lung-health-diseases/lung-disease-lookup/pulmonary-embolism/learn-about-pulmonary-embolism


 October 31, 2025
October 31, 2025