February 19, 2009 - The New England Journal of Medicine this week published the results from the SYNTAX trial, in which percutaneous coronary intervention (PCI) using the TAXUS Express2 Paclitaxel-Eluting Coronary Stent was compared to contemporary coronary artery bypass graft (CABG) surgery in patients with the most complex coronary artery disease (CAD).
Trial results at 12 months demonstrated no overall statistically significant differences between PCI and CABG in rates of death or myocardial infarction, although PCI patients were more likely to require a repeat revascularization (mostly additional PCI) than were CABG patients.
The SYNTAX trial is the first randomized, controlled clinical trial to compare these two treatments in patients with left main disease and three-vessel disease. These patient groups are typically treated with CABG and represent a population with far more complex anatomy and advanced disease than those studied in prior drug-eluting stent (DES) clinical trials.
“SYNTAX has provided the medical community with critical information on the management of patients with advanced and complex CAD,” said Ted Feldman, M.D., FSCAI, director of the cardiac catheterization lab at NorthShore University Health System in Evanston, IL, and a lead investigator of the trial. “While CABG may still be the preferred treatment in many patients with complicated disease, some patients may now be candidates for the less-invasive alternative offered by stents. These data will assist cardiologists in making treatment therapy decisions for these patients.”
The SYNTAX trial enrolled 1,800 patients in its randomized arm, using an innovative consecutive enrollment methodology. All patients were assessed by a multidisciplinary team including an interventional cardiologist and a cardiac surgeon. If both the cardiologist and surgeon felt they could offer equivalent complete revascularization, patients were randomized 1:1 into one of the two treatment strategies (PCI or CABG). If either the cardiologist or surgeon felt that one revascularization technique was the preferred treatment, then patients were not randomized, but were entered into the corresponding registry. Accordingly, patients in the PCI registry had been rejected for cardiac surgery, and patients in the CABG registry had been rejected for PCI.
The patients recruited in the SYNTAX trial are a unique study group in the PCI field, given their exceptionally complex anatomy and advanced disease. The average PCI-treated patient enrolled in SYNTAX received 4.6 stents. By contrast, the average number of stents implanted in a PCI patient in everyday practice is 1.5. Further evidence of the complex nature of PCI-treated patients enrolled in SYNTAX include 33 percent of patients with >100 mm stented length, 72 percent with bifurcations, 22 percent with total occlusions and 39 percent with left main disease.
The final one-year results published today showed similar safety for the two randomized groups, with a combined rate of all-cause death, stroke and myocardial infarction (MI) of 7.6 percent for PCI and 7.7 percent for CABG (p=0.98). The rate of stroke itself was significantly lower for PCI (0.6 percent for PCI as compared to 2.2 percent for CABG, p=0.003). Overall 12-month MACCE (all-cause death, stroke, MI and repeat revascularization), however, was significantly higher for PCI (17.8 percent versus 12.4 percent, p=0.002), due to more repeat revascularization in the PCI arm (13.5 percent versus 5.9 percent, p=0.001). Most repeat revascularizations in the PCI arm, however, were performed by additional PCI, with only 2.8 percent of PCI patients ultimately requiring CABG.
The SYNTAX trial broke new ground by scientifically defining a new measure for anatomical complexity - the SYNTAX Score - which characterizes vasculature based on lesion number, complexity and location. In fact, PCI patients in the lower one-third of raw SYNTAX Score results had similar 12-month combined MACCE rates to CABG patients (13.6 percent for PCI and 14.7 percent for CABG, p=0.71).
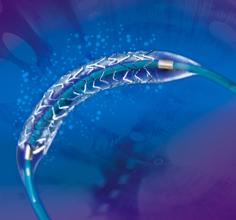
The TAXUS Express2 Paclitaxel-Eluting Coronary Stent System used in the SYNTAX trial has now been replaced by the Boston Scientific’s second-generation TAXUS Liberte Paclitaxel-Eluting Coronary Stent System, which has been approved for use in the U.S., Europe and Japan. This stent represents the company’s latest advance in drug-eluting stent technology, with substantially thinner struts and a more flexible cell geometry for improved deliverability, as well as uniform strut distribution designed specifically for more even drug elution.
For more information: www.bostonscientific.com


 January 15, 2026
January 15, 2026 









