August 29, 2011 — Recent data suggest post-operative outcomes of severe heart failure patients bridged short-term ventricular assist devices (VADs) to urgent heart transplantation are significantly worse than in patients bridged with conventional support. The data comes from the Spanish National Heart Transplant Registry.
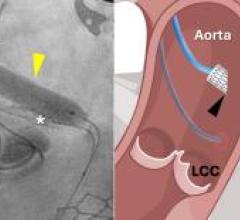
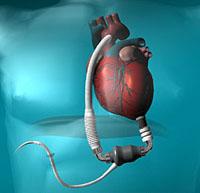
Spanish investigators led by Eduardo Barge-Caballero, M.D., and Marisa Crespo-Leiro, M.D., from the Hospital Universitario A Coruña conducted a multi-institutional retrospective study of 704 patients with critical heart failure. All patients also underwent urgent heart transplantation in 15 Spanish hospitals from January 2000 to December 2009. One hundred and seven patients had been supported with short-term VADs before transplantation, while the remaining 597 had been bridged with conventional therapy; that included intravenous inotropes, invasive mechanical ventilation and/or intra-aortic balloon pump (IABP). Implanted VADs were paracorporeal pulsatile-flow devices in 58 cases and extracorporeal continuous-flow ones in 47. Mean waiting list time was extremely short, around five days, a characteristic fact of the well-organized Spanish high-emergency organ procurement and allocation system.
Despite fairly similar pre-transplant clinical status and end-organ function, VAD bridged patients showed a higher incidence of severe surgical bleeding, longer bypass times and higher rates of primary graft failure than conventionally bridged patients, so as resulting in a significantly reduced post-transplant survival.
In Barge-Caballero´s opinion, “our data suggest that routine short-term VAD implantation in stable patients awaiting high-emergency heart transplantation should not be recommended, at least in countries with expected short waiting list times, as this strategy might compromise heart transplant outcomes”. For the main investigator of the study, “short-term VAD support as a bridge to high-emergency heart transplantation should be reserved for critically ill patients with a deteriorating hemodynamic status, in which conventional therapy is not enough to ensure adequate peripheral perfusion and to avoid irreversible end-organ damage”.


 February 06, 2026
February 06, 2026