
The Gore Tigris is a dual-component stent with a unique fluoropolymer / nitinol design.

A close up view of the polymer links that differentiate the Tigris from other peripheral stents. The polymer is said to be more flexible and less prone to stent strut fractures.
August 2, 2016 —The U.S. Food and Drug Administration (FDA) granted market clearance for W. L. Gore & Associates’ Gore Tigris Vascular Stent, a dual-component stent with a unique fluoropolymer / nitinol design. The Gore Tigris device, which gained CE mark approval in 2011, is a third generation, self-expanding stent. The device was designed explicitly to improve anatomical conformability with the natural movement of the knee when treating peripheral artery disease (PAD).
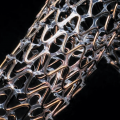 The newly-approved Gore Tigris Vascular Stent uses a dual component structure, made from a single-wire nitinol stent with flexible and biocompatible fluoropolymer interconnections. The stent has been designed to weather biomechanical forces (extension, compression, flexion and torsion) without fractures, even in the most complex anatomies, namely in the superficial femoral artery (SFA) and proximal popliteal artery (PPA). In the U.S. clinical study that supported FDA approval, the Tigris was found to have zero fractures, while the control arm devices experienced a 27 percent fracture rate.
The newly-approved Gore Tigris Vascular Stent uses a dual component structure, made from a single-wire nitinol stent with flexible and biocompatible fluoropolymer interconnections. The stent has been designed to weather biomechanical forces (extension, compression, flexion and torsion) without fractures, even in the most complex anatomies, namely in the superficial femoral artery (SFA) and proximal popliteal artery (PPA). In the U.S. clinical study that supported FDA approval, the Tigris was found to have zero fractures, while the control arm devices experienced a 27 percent fracture rate.
“The Tigris Vascular Stent has an innovative design that is very different from any of the other nitinol stents that we currently use. The extreme flexibility of this stent makes it well suited for the superficial femoral artery and proximal popliteal artery, and the delivery system is highly accurate. The precision offered by this flexible, dual component device allows for easy insertion and predictable clinical outcomes, even in challenging anatomy,” said John R. Laird, M.D., an interventional cardiologist in Davis, Calif.
The Gore Tigris also features Gore's CBAS Heparin Surface, a lasting heparin bonding technology designed to resist thrombus formation, a problem common in both bare metal and drug-eluting stents. End-point covalent bonding keeps heparin anchored to the stent surface, while the bioactive site remains free to interact with the blood to help prevent clotting.
Gore said the evolution of peripheral stenting over the past decade has allowed for broader adoption of endovascular therapy for treating PAD. When physicians began placing stents in the SFA, they were limited by first generation stent designs that had longitudinal metal connections, which led to arterial stiffening, high fracture rates and poorer clinical outcomes. Improvements in second generation devices introduced helical interconnections to improve flexibility, however, their success in high flexion vessels, like the distal SFA and PPA, was still limited.[1] The introduction of third generation stents, including the Gore Tigris Vascular Stent, allow for better adherence in some of the more intricate vessels in the body.
PAD is prevalent in older populations, a rapidly growing demographic in developed countries. In the U.S. alone, approximately 8 to 12 million people suffer from some form of PAD. The disease can manifest in mild symptoms such as chronic leg pain, and more serious complications include poor wound healing, increased risk of stroke, and amputation. Endovascular treatment, via angioplasty and stenting of a blocked artery, is designed to treat PAD without the complications that can accompany open surgery.
For more information: www.goremedical.com/tigrisna
Reference:
1. Thaveau F, Méteyer V, LeJay A, Chakfé N. “Latest generation of conforming dual component stent.” Greenhalgh RM, ed. Charing Cross 2016-Vascular & Endovascular Challenges Update. 2016 ed. Fulham, London, United Kingdom: BIBA Publishing; 2016:423-428.


 November 14, 2025
November 14, 2025 









