April 8, 2020 – The scientific community is learning more about the impact and interaction of cardiovascular diseases with novel coronavirus (COVID-19, SARS-CoV-2), including the impact of drug therapies being used and their negative cardiovascular impact. Together, the American Heart Association (AHA), the American College of Cardiology (ACC) and the Heart Rhythm Society (HRS) April 8 jointly published a new guidance, “Considerations for Drug Interactions on QTc in Exploratory COVID-19 (Coronavirus Disease 19) Treatment,” to detail critical cardiovascular considerations in the use of hydroxychloroquine and azithromycin for the treatment of COVID-19.[1]
This guidance is published in Circulation, the journal of the American Heart Association, the Journal of the American College of Cardiology (JACC), and Heart Rhythm Journal, the official journal of the HRS.
Hydroxychloroquine and Azithromycin Pose Serious Health Risks
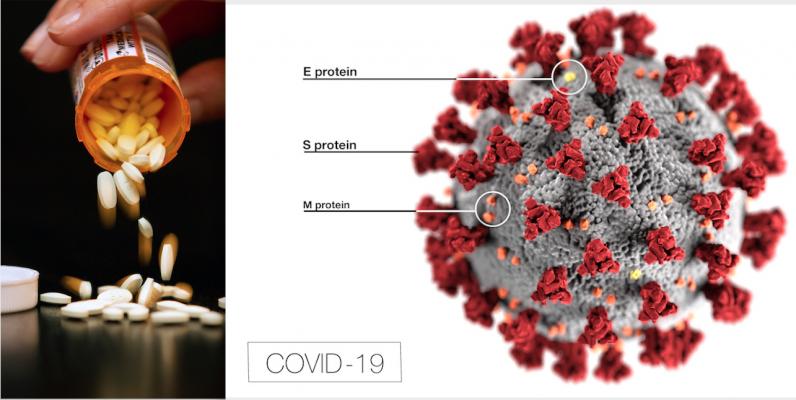
The antimalarial medication hydroxychloroquine and the antibiotic azithromycin are currently gaining attention as potential treatments for COVID-19, and each have potential serious implications for people with existing cardiovascular disease. Complications include severe electrical irregularities in the heart such as arrythmia (irregular heartbeat), polymorphic ventricular tachycardia (including Torsade de Pointes) and long QT syndrome, and increased risk of sudden death. The effect on QT or arrhythmia of these two medications combined has not been studied.
The AHA, the ACC and the HRS guidance for health care professionals includes additional mechanisms to reduce the risk of arrhythmias. Steps outlined:
• Electrocardiographic/QT interval monitoring;
• Withhold hydroxychloroquine and azithromycin in patients with baseline QT prolongation (e.g. QTc ≥500 msec) or with known congenital long QT syndrome;
• Monitor cardiac rhythm and QT interval; withdrawal of hydroxychloroquine and azithromycin if QTc exceeds a present threshold of 500 msec;
• In patients critically ill with COVID-19 infection, frequent caregiver contact may need to be minimized, so optimal electrocardiographic interval and rhythm monitoring may not be possible;
• Correction of hypokalemia >4mEq/L and hypomagnesemia >2mg/dL; and
• Avoid other QTc prolonging agents whenever feasible.
The statement also includes a table rating potential adverse cardiac events of medications currently being repurposed for COVID-19 treatment, such as chloroquine and lopinavir/ritonavir (antimalarial and antiviral agents, respectively).
“The urgency of COVID-19 must not diminish the scientific rigor with which we approach COVID-19 treatment. While these medications may work against COVID-19 individually or in combination, we recommend caution with these medications for patients with existing cardiovascular disease,” said Robert A. Harrington, M.D., FAHA, president of the American Heart Association, Arthur L. Bloomfield Professor of Medicine and chair of the department of medicine at Stanford University.
“We are united in our mission to achieve optimal, quality care for our patients, and we must continue to be vigilant in assessing the potential complications of all medications during this crisis,“ stated Athena Poppas, M.D., president of the American College of Cardiology, professor of medicine at Brown University and chief of cardiology and director of the Lifespan Cardiovascular Institute at Rhode Island, the Miriam and Newport hospitals in Providence, Rhode Island.
“Given the potential for increased risks related to combinations of medications that prolong the QT interval, we urge careful consideration to ensure patients with cardiovascular disease or others at increased risk can be monitored appropriately,” stated Andrea M. Russo, M.D., president of the Heart Rhythm Society, director of Electrophysiology and Arrhythmia Services at Cooper University Hospital, director of the CCEP Fellowship Program, and professor of medicine at Cooper Medical School of Rowan University in Camden, New Jersey.
The statement is also co-authored by Dan M. Roden, M.D., C.M., interim division chief of cardiovascular medicine, senior vice president for personalized medicine, faculty of the clinical cardiac electrophysiology program, Sam Clark Chair in Experimental Therapeutics, professor of pharmacology and professor of biomedical informatics at Vanderbilt University in Nashville, Tennessee.
UPDATED JUNE 15, 2020 — FDA Revokes Emergency Use Authorization for Chloroquine and Hydroxychloroquine for COVID-19
For more information: HRSonline.org, acc.org
Related COVID-19 Therapy Content:
VIDEO: Overview of Hydroxychloroquine and FDA Warning in its use to Treat COVID-19 — Interview with Marianne Pop, Pharm.D.
FDA Reports of Deaths and Injuries From Use of Antimalarial Drugs in COVID-19 Patients
VIDEO: Why QT-prolongation Occurs in COVID-19 Patients on Hydroxychloroquine — Interview with Andrew Krahn, M.D.
COVID-19 Hydroxychloroquine Treatment Brings Prolonged QT Arrhythmia Issues
No Evidence Supporting Discontinuing RAAS Inhibitors in COVID-19 Patients in NEJM Article
ESC Council on Hypertension Says ACE-I and ARBs Do Not Increase COVID-19 Mortality
FDA Approves ECMO to Treat COVID-19 Patients
Cardiology Related COVID-19 News and Videos
VIDEO: Cardiologists Manage Trial Testing if Hydroxychloroquine Protects Clinicians From COVID-19
First Large-scale U.S. Study on Hydroxychloroquine COVID-19 Prophylaxis Begins in Detroit
VIDEO: What Cardiologists Need to Know about COVID-19 — Interview with Thomas Maddox, M.D.
Reference:


 July 31, 2024
July 31, 2024 









