Percutaneous mechanical thrombectomy (PMT) devices are increasingly being used to remove clots from coronary and peripheral vessels. They offer a faster treatment option than using traditional systemic thrombolytic (lytic) or catheter-directed thrombolysis (CDT).
“These are expensive cases and very taxing on the doctor’s resources, the hospital’s resources and the patient’s resources,” said Robert A. Lookstein, M.D., FSIR, FAHA, associate professor of radiology and surgery, associate director of interventional radiology, Mount Sinai Medical Center, New York. For these reasons, several interventional thrombectomy devices were introduced in the past 10 years.
“I think the medical device community really stepped up in developing new devices,” Lookstein said. “The purpose of these devices was to obviate the need for thrombolytics, cut the amount of time it takes to treat these patients, prevent the need for sending these patients to the intensive care unit for monitoring and to reduce the complication rates. Modern techniques allow these cases to be finished quickly and more safely than ever before. I have not had to treat a patient with an overnight infusion in three years, because I have adopted these more aggressive techniques.”
Issues With Lytic Therapy
At the start of the decade, lytics, primarily tissue plasminogen activator (tPA), were the standard of care for acute thrombosis. The drugs were delivered in an intravenous drip or directly to the clot using multiside-hole infusion catheters. As the clot dissolved, the catheter was advanced further down the leg. However, it took up to three days to treat patients, said Peter Soukas, M.D., director of vascular medicine and assistant professor of medicine, Tufts University School of Medicine, St. Elizabeth’s Medical Center, Boston.
He performs about 500 peripheral interventional thrombectomy cases per year, including arterial, deep vein thrombosis (DVT) and pulmonary embolism (PE). He said the use of tPA alone has a 30 percent complication rate. Soukas explained 10 percent of patients suffer major bleeding events (including about 1.5 percent intracranial bleeds). About 20 percent of patients suffer minor bleeding events.
“Minimizing bleeding complications is as important as saving the limb,” Soukas said.
The Rise of Combination Therapy
While several thrombectomy devices were developed in the early 2000s, they are not the final answer. “The thrombectomy catheters are not terribly effective on their own,” Lookstein said.
About six years ago, many centers started experimenting with lytics in combination with these devices. Today, Lookstein said this combination therapy is the standard of care in patients with peripheral thrombosis.
St. Elizabeth’s Medical Center began using tPA with the Covidien (formerly Bacchus Vascular) Trellis and the Ekos ultrasound-enhanced infusion catheter.
“These devices make it safer, faster and more cost-effective to treat these patients,” Soukas said, adding they use much less tPA than infusion catheters alone. “Less tPA means less likelihood of major bleeding complications.”
Thanks to these devices, he said the number of bleeding complications is down significantly from the rates 10 years ago.
“It is a huge cost savings for the hospitals and payers, and it is huge for increasing patient satisfaction,” Lookstein said.
“When used properly in combination with thrombolytic drugs, these thrombectomy catheters can shorten treatment times dramatically,” Lookstein said.
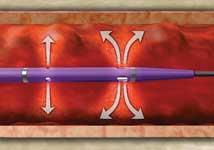
The AngioJet Catheter
One of the most versatile thrombectomy systems is the Medrad/Possis AngioJet, which combines aspiration, lytic infusion and high-speed jets of saline to quickly break down thrombus. It has indications for peripheral arteries, peripheral veins, coronary arteries, bypass grafts and dialysis access grafts and fistulas. It has a pulse delivery feature to infuse tPA directly into clots. Its thrombectomy mode uses high-velocity saline jets (10,000 psi) at the tip to break up thrombus and aspirate it at the same time.
Ali Amin, M.D., a vascular surgeon at The Read Hospital and Medical Center in Reading, Pa., prefers the AngioJet over other devices because it offers different-sized tips to work in various vessels. He said the indications for coronary and peripheral vessels make it ideal for cath labs that perform both procedures.
When treating clots with the AngioJet, Amin pulses tPA directly into the clot first and waits 40 to 50 minutes before using the full action of the device to break apart and aspirate the clot.
“The longer you allow it to sit, the more contact the clot will have with the tPA and the easier it is to remove,” Amin said. “If you allow the tPA to penetrate, the run time [for the AngioJet] is much shorter.”
“The AngioJet is very good at sucking out an acute clot,” Soukas said. However, the longer a clot solidifies, the more difficult he finds the device to use. He uses the AngioJet for clots that are less than 24 hours old. “We still use it and it is still a very good device. But if a clot is more than a day old, we usually will not use it as the initial primary therapy,” Soukas said.
Lookstein disagrees and will use the AngioJet for clots up to two weeks old. He agrees clots solidify more with each passing day, but can still be treated with thrombectomy up to about 14 days. After that time, they are considered chronic thrombus and are more difficult to treat.
Fans of the AngioJet say the aspiration feature prevents distal embolization. Critics say the device can still allow emboli to escape downstream.
“It can work very effectively for acute clots, but its Achilles heel is distal embolization,” Soukas said.
Another criticism of AngioJet is that pulsing tPA into the clot allows the drug to flow throughout the body, which may lead to bleeding complications. However, many who regularly use the device disagree.
“The fear of the tPA becoming systemic with the AngioJet is over blown,” Amin said. “You are injecting the tPA into the clot and then aspirating the clot along with the tPA.”
Removing Arterial Clots
“Time is really against you with an arterial clot. You also need to remove as much clot as possible [to prevent distal embolization],” Soukas said. “You really are racing against time, and anything you can do to get that artery open and reduce these complications is what you want to use.”
Lookstein uses both the AngioJet and Trellis devices, but said AngioJet works best in arterial cases. He feels it is more versatile with its several different-sized tips.
Amin said the Trellis works well in peripheral bypass grafts. But, it does not work as well in native vessels that are heavily stenosed, which is where he said the AngioJet works best.
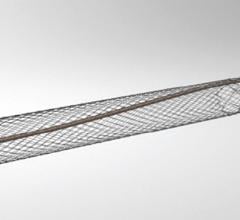
The Trellis Device
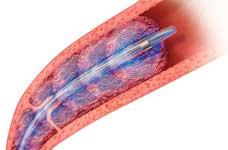
The Trellis device uses two balloons to occlude a vessel segment, which is then flooded with tPA. An oscillating wire between the balloons helps mechanically break up the clot, which is then aspirated prior to the balloons being deflated. It comes with treatment area lengths of 10, 15 and 30 cm.
Since the tPA is concentrated in a confined space, Soukas said it works more effectively than when it is diluted in the blood. He said most treatments take 15 minutes before the clot can be aspirated. He uses it primarily for DVT in the femoral and iliac veins. Due to its 8 French size, it cannot be used below the knee.
Amin said the disadvantage of Trellis is the oscillating wire could possibly damage venous valves. However, he said its advantage is it contains the tPA and prevents it from flowing systemically.
“The Trellis-8 is usually reserved for venous thrombus, and we use the Ekos for arterial thrombus,” Soukas said. He said the main difference in use is based on the size of the devices. Trellis uses an 8 French catheter and the Ekos a 6 French catheter. “When you are giving someone tPA, not surprisingly, we don’t like to use the larger catheters in arteries,” he explained.
Recently, the Trellis-6 became available for treating proximal arterial clots.
Soukas frequently uses the Trellis, Ekos and AngioJet in combination. “With the Trellis, we can treat most of the clot burden and treat the residual clot with Ekos,” he said. “AngioJet is also used for mopping up after treating a large clot with other devices. I see them as complementary, not competitive, tools to remove thrombus and restore flow.”
Ultrasonic Clot Busting
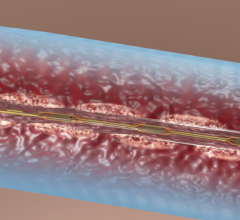
Ekos Corp. developed a catheter that combines targeted delivery of lytics with an ultrasound catheter to help the drug penetrate the thrombus. Last November, Ekos released its newest version, the EkoSonic Mach4e with Rapid Pulse Modulation (RPM). The system reportedly uses less lytic and achieves faster removal of arterial and venous clots. The device automates a number of manual steps, making it easier to use than previous models.
“The reason why the Ekos is so helpful is because its low-energy ultrasound helps to diffuse the lytic into the clot, helping it to dissolve the clot,” Soukas said. Ekos said the ultrasound waves help increase drug uptake by the clot and uses 50-70 percent less lytic drug.
“The Ekos is an excellent technology that allows for reliable removal of thrombus,” Lookstein said. “But I have not seen data showing it can reliably remove all the thrombus in complex cases within 24 hours.”
However, he said with further refinement the Ekos treatment times will likely drop.
Amin uses both the Ekos and Angiodynamics infusion catheters. He said they are best suited for mopping up veins to eliminate residual clots after use of thrombectomy devices. He also uses them to treat chronic thrombus that has been in smaller vessels for weeks. It takes longer for tPA to dissolve established thrombus in these vessels.
Soukas found Ekos is also very effective at removing thrombus from inside covered stents, cleaning them out within a few hours.
Gaining Access to Thrombosed Vessels
Since an occluded vessel cannot be clearly visualized with angiography, ultrasound can be used as an alternative, said Peter Soukas, M.D., director of vascular medicine and assistant professor of medicine, Tufts University School of Medicine, St. Elizabeth’s Medical Center, Boston. He uses ultrasound to guide access, especially when introducing a catheter into an occluded vein.
The ultrasound can help navigate to the intended vein, rather than inadvertently puncturing the popliteal artery.
He noted occluded vessels may not have any blood flow, so it is not always as apparent when you are inside the vessel, as it is with a vessel that is free-flowing.




 November 21, 2022
November 21, 2022