The high cost of patient care is influencing many decisions in today’s healthcare marketplace. The expense of treating the estimated five million Americans who suffer from heart disease alone is a staggering $26.7 billion dollars annually and growing.
One approach to controlling such exorbitant costs is applying very targeted care. If you look to the business community, it spends a lot of time defining goals and objectives for virtually every aspect of growth and profit. Perhaps the pursuit of specific goals in the various business enterprises stems from an age-old axiom that only that which can be adequately defined has any hope of ever becoming a reality. It may seem to be a “stretch” of sorts to lump hemodynamic monitoring into a similar vein. However, monitoring derives much of its credence from measured values, quantitative analysis and myriad methods for displaying raw data and information. So how can hemodynamic monitoring achieve targeted care?
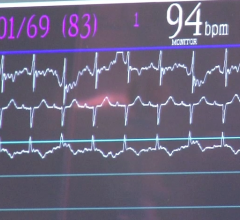
There has been a lot of discussion lately about the varying degrees of dynamic and static types of hemodynamic monitoring and their various effects and affects on both the quality of patient care and the cost of patient care.
All of the latest arguments, both for and against differing methodologies, protocols and technological usages, can be boiled down to a few key determining factors. Ultimately, the ability to track physiologic changes is determined by many factors, including the type of patient represented within the clinical setting, the type of technology used and defined protocols agreed upon.
Following Doctors Orders
Patients who fail to follow their physicians’ recommendations, for example, are difficult to monitor and often become a chronic financial burden to the healthcare system.
Despite the ubiquity and frequency of acute decompensated heart failure, there are few available techniques to anticipate and correct decompensation. In this case, device-based diagnostic monitoring with an implantable cardioverter defibrillator for the prevention of sudden cardiac death and biventricular pacing for dyssynchrony in heart failure (HF) refractory to medical treatment are expanding in the HF population. Therefore, device-based diagnostic monitoring strategies have the potential to identify patients at risk for decompensation and decrease costly healthcare uses.
Due to the benefits of implantable hemodynamic monitoring devices to both the patient and the cost-conscious administrator, these types of solutions are on the rise and will likely continue to infiltrate the world of hemodynamic monitoring.
Trend Toward Noninvasive Devices
The drawback with invasive procedures is that not only do they cause discomfort for the patient who has to undergo the ordeal of having a pulmonary artery catheter (PAC) inserted for heart monitoring, but the expense associated with such an invasive procedure is compounded by the considerable risk of complications.
Advances in technology, however, are changing the clinical landscapes in the emergency department and intensive care unit (ICU) from a reliance on invasive therapies to increased use of noninvasive monitoring devices. With less invasive technologies for hemodynamic monitoring, insertion of the catheter may be completed by a nurse outside of the ICU, saving money and requiring less time in the ICU.
One example of this is the recent introduction of the Hickey Cardiac Monitoring System (HCMS). The device consists of a small two-balloon catheter and a monitor. Its small catheter is inserted down the throat, positioned in the esophagus and inflated. Changes in cardiac function then create subtle pressure changes in the balloons, which are relayed to the monitor. The HCMS is reportedly comfortable enough to allow a patient to continue to eat, drink and sleep even with it inserted, and the procedure is noninvasive enough that a patient’s stay in the ICU may be shorter.
The Plethysmograph Variability Index (PVI) is a new noninvasive measurement, developed by Masimo, a pulse oximetry company, that quantifies changes in the plethysmographic waveform derived from pulse oximetry. PVI displays a numeric representation of the changes to the pleth waveform on the pulse oximeter and allows clinicians to track and trend these changes over time as well as a Diagnostic Plethysmograph that maintains the morphology of the true pleth for clinicians to view.
As more noninvasive measurements are validated, they can be incorporated into more targeted care in a cost-effective manner.
IT Streamlines Monitoring
Another win-win for both sides of the treatment equation is technology that allows patients to be sent home to be with family while simultaneously monitored for critical events. IT solutions can help improve both patient outcomes and the underlying, sometimes elusive, patient satisfaction goals garnered by hospitals and healthcare systems nationally.
Technologies that allow for the detailed collection and use of patient data promote both the quality of the healthcare delivered and lower these costs. With the increasing volume of cardiovascular studies, workflow efficiencies become more critical to patient care and the bottom line. Gaining efficiencies in collecting hemodynamic data and producing reports may be achieved through systems such as McKesson’s Horizon Cardiology Hemo, a hemodynamic monitoring system, and its cardiovascular image and information solution to streamline the monitoring process.
By automating the recording and monitoring of patient’s vital signs and data during a cardiac catheterization procedure, cardiologists can expedite charting and final reporting, view reports in real-time and query the database for decision support. Plus, these systems allow cardiologists to access information remotely in order to provide care and monitor patients regardless of whether they are in the hospital, their offices or at home.
Reach Goals with Targeted Protocols
There is a trend away from broadly applied protocols and toward more targeted monitoring to meet the specific needs. This school of thought believes that highly targeted protocols should be used as part of a treatment protocol of proven efficacy because the delivery of protocolized, goal-directed therapies improves patient outcomes.
One of the key ways to derive additional benefit from the hemodynamic monitoring arena is to develop treatment goals associated with each element of this technology usage. Clinical goals tied to technological capabilities can produce significant results for both the clinician and the cost-conscious administrator.
As with business goals, hemodynamic usage goals should be adequately defined and measured to secure the objectives of patient care improvement as well as reliable cost containment.


 January 13, 2026
January 13, 2026