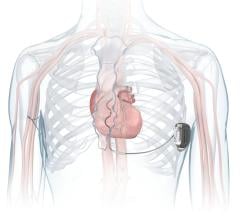
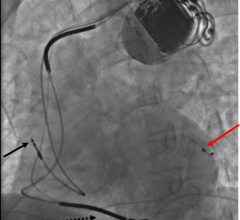
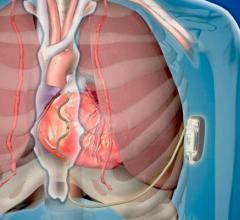
Without a doubt, implantable cardioverter defibrillators (ICD) and cardiac resynchronization therapy devices with integrated defibrillators (CRT-D) have made a positive impact on millions of individuals by slowing the progression of heart failure and giving patients better health and quality of life. Studies have shown that earlier intervention in heart failure patients can significantly decrease hospitalization rates and many patients now receive cardiac rhythm management (CRM) devices at a younger age than in the past.[1] In fact, between 35 and 45 percent of patients with an ICD of CRT-D are under the age of 65. Despite these clear benefits and the work that CRM device manufacturers have done to enhance their products, there are still strides to be made, especially in the battery life of devices.
Historically, ICT and CRT-D devices have needed to be replaced every three to seven years as the device's battery life deteriorates. Consequently, it is not unusual for patients to require several device replacements over their lifetime meaning additional costly procedures and increased risk of complications with each procedure. As the baby boomer population in the United States continues to age, and the average life expectancy in the United States increases to 76 years for men and 81 years for women, the number of patients who would benefit from a CRM device will grow exponentially. For the average patient whose CRT-D or ICD device lasts three to five years, this could result in two to four device change-outs over their lifetime.
Complications Related to Change-Outs
Device change-outs can often be complex, costly and are associated with increased mortality. In a recent study from Leiden University, 9 percent of patients experienced complications following a device change-out.[2] Additionally, there is an increased need for re-intervention associated with every consecutive replacement.
Other studies have found that the risk of infection also increases for patients who have more frequent device change-out, from less than 1 percent following the initial implant to 2-7 percent following device replacement.[3, 4, 5] When a device infection occurs, the American Heart Association (AHA) and Heart Rhythm Society (HRS) recommend removal of both the device and leads.[6, 7]
Improving Battery Life
Many device manufacturers have begun to capitalize on improved battery technology to extend the lifecycle of their current devices and also are creating new products that could potentially last twice as long. Existing devices have up to twice the battery capacity as older models, are as energy-efficient as a pacemaker, and do not have the mid-life charge time issues associated older battery chemistry. Despite this, more often than not, devices do not last as long as projected. In fact, Medtronic’s November 2011 Product Performance Report showed that only 40 percent of CRT-Ds released into the market in 2007 were still in service after 4.4 years.[8]
CRM patients are generally told to expect that the battery life of their device is about five years for CRT-D devices and as many as seven or eight for ICDs. Devices with additional features such as continuous pacing, remote monitoring and anti-tachycardia pacing therapy during charging can exhaust batteries more quickly.
Costly Replacement
To illustrate the impact of a longer battery life, imagine a 54-year-old heart failure patient who received a device with a 4.4-year battery life. This patient would need five device replacements by the age of 80, requiring a total of six surgeries. According to the ICD registry, the approximate procedure and device replacement cost is about $37,000,[9] excluding physician and anesthesia fees. The six surgeries this patient would require could cost more than $220,000 and also require out-of-pocket expenses. If this patient received a device that had double the battery life of approximately eight years, this would reduce the number of surgeries required and associated costs by half.
For the next generation of patients, the cost difference between a device that lasts four to five years versus eight to 10 years would be substantial.[10, 11] A study at the Cleveland Department of Veterans Affairs Hospital concluded that many of the costs associated with device replacements could have been avoided with longer battery life.[12] In fact, the study estimated that the potential cost savings for devices lasting seven to nine years would be $190 million to $292 million in 2005 Medicare dollar costs to the healthcare system over a 15-year period.[11]
New Battery Technology
Since most CRM device manufacturers develop and produce their own batteries and much of the performance information is proprietary, it can be difficult to measure how long certain batteries last. In general, new devices that utilize a lithium manganese dioxide battery chemistry do not have the mid-life charge time issues associated with lithium silver vanadium oxide battery chemistry.
The only measurement is from projections of longevity and reliability from each manufacturer’s device warranties. One device manufacturer, Boston Scientific, began working on its current battery technology in 2002 and now has a 10-year-warranty on its ICD and CRT-D systems. These batteries have nearly twice the capacity of some devices while still requiring the same low-power consumption as a pacemaker.
The effort by device manufacturers to develop technology to increase longevity and effectiveness of their products is commendable and promises to significantly improve the health of millions of patients in the United States. In the coming years, the continued growth and aging of our population will both increase the demand for treatment with implantable cardiac rhythm devices and stretch our ability to pay for care. Toward solving this, we must continue to improve clinical quality not just to provide a better future for patients, but to control costs so that we are able to meet the increased demand.
Editor’s note: Mike Vintges is the vice president, physician preference, sourcing operations at Novation. The company provides healthcare supply chain expertise and contracting for the more than 65,000 members of VHA Inc. and UHC, two national healthcare alliances, and Provista LLC. It provides alliance members with sourcing services, as well as information and data services. www.novationco.com
References:
1. AJ Moss; Hall, WJ; Cannom, DS; Klein, H; Brown, MW; Daubert, JP; et al. “Cardiac-resynchronization therapy for the prevention of heart-failure events.” NEJM, 2009; 361(14):1329-38.
2. Borleff CJ, Thijssen J, Mihaly K, van Rees JB, van Erven L, et al. “Recurrent implantable cardioverter-defibrillator replacement is associated with an increasing risk of pocket-related complications.” PACE 2010; 33: (1013-19).
3. Paul A. Gould, Lorne J. Gula, Raymond Yee. “Cardiovascular implantable electrophysiological device-related infections: a review.” Current Opinion in Cardiology 2011; 26:6–11. High-risk is defined as QRS width ? 130 ms, LVEF ? 30 percent, and LBBB.
4. Peterson PN, Daugherty SL, Wang Y, Vidaillet HJ, Heidenreich PA, Curtis JP, Masoudi FA, et al. “National Cardiovascular Data Registry. Gender differences in procedure-related adverse events in patients receiving implantable cardioverter-defibrillator therapy.” Circulation 2009; 119:1078-1084.
5. Poole, JE; Gleva, MJ; Mela, T; et al. “Complication rates associated with pacemaker or implantable cardioverter-defibrillator generator replacements and upgrade procedures results from the REPLACE Registry.” Circulation 2010; 122: 1553-1561.
6. Klug D, Balde M, Pavin D, Hidden-Lucet F, Clementy J, Sadoul N, Rey JL, et al. “Risk factors related to infections of implanted pacemakers and cardioverter-defibrillators: Results of a large prospective study.” Circulation 2007; 116: 1349-1355.
7. Wilcoff BL. “How to treat and identify device infections.” Heart Rhythm 2007; 4: 1467-1470.
8. www.medtronic.com/productperformance/model/C154DWK-concerto-crt-d-dr.html. Accessed Nov. 2, 2011.
9. Sohail MR, Henrikson A, Braid-Forbes MJ, et al. “Mortality and cost associated with cardiovascular implantable electronic device infections.” Arch Intern Med, published online Sept. 12, 2011.
10. ICD Registry June 2010 update, full year 2009.
11. Saxon LA, Boehmer JP, Day JD, et al. “Survival after ICD implant and incidence of device therapy in patients less than 30 years old: The ALTITUDE study group.” Presented at ESC 2011. http://spo.escardio.org/eslides/view.aspx?eevtid=48&fp=2802
12. Ramachandra I. “Impact of ICD battery longevity on need for device replacements – insights from a Veterans Affairs database.” PACE 2010; 33: 314-319.

 January 13, 2026
January 13, 2026