February 27, 2015 — Four-month-old Jackson Lane has a large scar that looks like a giant zipper down the center of his chest, the result of undergoing a lifesaving surgical procedure at just five days old to repair an extremely rare heart condition.
Elyse Lane was 20 weeks pregnant in June 2014 when she went for a routine fetal exam at her doctor’s office in Phoenix. She and her husband Andy, formerly a Major League Baseball coach with the Chicago Cubs, knew they were having a boy and, based on earlier appointments, they didn’t expect any surprises at this one. But the ultrasound found there was something wrong with the baby’s heart.
The first specialist they saw told them the baby was missing his pulmonary valve and that the pulmonary artery was massive. The artery was so large – 10 times the size it should have been – that it was significantly and dangerously impeding the growth of his airway. Their doctor told them they should consider terminating the pregnancy. Even if the baby made it to term – and the doctor cautioned that it wasn’t clear he would – he likely would need mechanical assistance to breathe.
“When we asked what the outlook was and what his life expectancy might be, we got vague answers,” Elyse said. “It was heartbreaking.”
Two days later, they took a redeye flight to Boston in search of second opinion. There, a specialist told them their baby had a condition called tetralogy of Fallot, a rare heart defect affecting blood and oxygen flow. The baby’s condition was complicated by the fact that he was also missing his pulmonary valve. But the doctor also gave the distraught parents their first glimmer of hope. The baby appeared strong and active in utero and, if he made it to term, there was a surgeon who could fix the problem not too far from their Arizona home: Frank Hanley, M.D., cardiothoracic surgeon at Lucile Packard Children’s Hospital Stanford and Stanford Children’s Health.
After contacting Hanley, they later came to Palo Alto to discuss an intricate and complex repair. The baby’s rare condition was extremely severe but Hanley wouldn’t know how quickly his team needed to operate – somewhere between hours and weeks – until after birth and after they determined how compromised his breathing was. The most important thing the couple could do was to try to deliver the baby as close to term as possible. They went back to Arizona and waited.
“Once we met Dr. Hanley, I knew everything was going to be okay,” said Andy. “We just fed off his confidence. He told us: ‘I’ve done this before and I can do this again.’”
When Elyse was 36 weeks pregnant, she and Andy packed their bags and flew back to California, expecting to spend the last four weeks of her pregnancy near Lucile Packard Children’s Hospital, where she would deliver the baby and Hanley would perform the surgery. Two days later, however, with the baby’s heart rate fluctuating wildly, doctors told the Lanes they needed to induce labor.
Six-pound, 5-ounce Jackson Lane arrived at 10 p.m. on Oct. 10 – nearly four weeks early – in a room filled with a team of 13 doctors, nurses and other care providers. Jackson arrived “worst-case scenario,” said Hanley – unable to breathe on his own. The enlarged pulmonary artery had severely compressed his bronchial tubes and he was whisked away to the neonatal intensive care unit, where he was placed on a ventilator. Even with the help of a ventilator, he was put on full life support and hooked up to an extracorporeal membrane oxygenation (ECMO) system to take over the work of the lungs and sometimes the heart.
“Jackson’s presentation was about as dramatic as you can get,” said Hanley, also the Lawrence Crowley, M.D., professor in child health and a professor of cardiothoracic surgery at Stanford University School of Medicine. “A case of this severity only comes around once every four or five years.” Hanley decided he’d need to perform the surgery soon because the baby couldn’t breathe on his own.
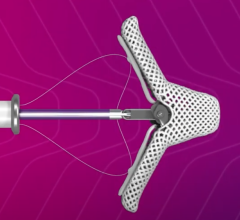
When he was just five days old, Jackson underwent a 13-hour operation that would save his life. Hanley and his team did a complex overhaul of Jackson’s heart: they inserted a pulmonary valve, reduced the size of Jackson’s right pulmonary artery, and enlarged his small, disconnected, left pulmonary artery. Hanley also used an innovative and intricate LeCompte maneuver, which altered the pathway of Jackson’s right and left pulmonary arteries from the back of the heart and aorta to the front. The double repair technique connects the left ventricle to the aorta and the right ventricle to the pulmonary artery using a technique that does not require an extracardiac conduit. This gave his severely compromised bronchial tubes room to grow and remodel after surgery was over.
“The benefit of moving it from behind to in front is that it takes the pressure off of the breathing tubes,” said Hanley. “It’s like driving a car; there are different routes you can take to get to the same destination. As long as the pulmonary arteries are re-routed in unobstructed fashion, there is no downside to having it in front of the aorta.”
Incredibly, Jackson and his parents left the hospital just after Thanksgiving when their newborn was just 7 weeks old – four months earlier than anyone expected. Because of the surgery, Jackson’s airway tubes were wide open and he was breathing normally.
Other than a few tune-ups – he’ll need to have a heart valve replaced as he gets bigger – Jackson is now expected to have a long and normal life.
For more information: www.stanfordchildrens.org




 December 24, 2025
December 24, 2025