Getty Images
In a room of 20 people, it’s likely that about 10 of them, or half, will presently have some form of cardiovascular disease (CVD).
CVD is among the most prevalent diseases in the U.S., and strokes and other CVDs are on the rise globally. One report projects a 50% increase in stroke-related deaths by 2050, with 10 million dying annually. Atrial fibrillation (AFib) cases have also surged, doubling from 28.3 million in 1990 to 56.7 million in 2019. This rise exacerbates the burden on overstretched cardiologists, who are facing a multitude of challenges like clinician shortages, complex workflows, administrative burden, poor patient adherence, health disparities and cost pressure.
Addressing rising CVDs in a way that also alleviates the cardiologist’s burden requires evolving the cardiology practice of today into the ‘cardiology clinic of the future’ — a bold new operating model that harmonizes virtual care experiences, workflow efficiency and personalized care. Let's journey through the cardiology clinic of the future and chart an actionable path that empowers healthcare teams to begin this transformation in their practices today.
Defining the "Cardiology Clinic of the Future"
What does the cardiology clinic of the future look like? Following are a few characteristics that distinguish the next evolution of the cardiology practice:
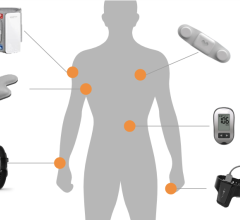
- Enthusiastic use of technology: The cardiology clinic of the future overcomes fear of adoption and embraces technology as a force multiplier for operational efficiency and clinical outcomes. This includes artificial intelligence (AI), remote monitoring, virtual care, and other emerging technological advancements.
- Clinical empowerment: In the clinic, technology abounds but is not a panacea. Instead, the clinician serves as the chief enabler of exceptional cardiac care. Technological investments are therefore focused on empowering clinicians to make more informed decisions faster and more proactively, spending a larger portion of their time on clinical tasks (as opposed to administrative or routine aspects of care).
- Rich data-driven diagnostics: Because the clinic embraces, rather than resists, technology-enabled change, it has more data at its disposal than traditional clinics. But more than possessing a glut of data, it transforms this data into action, actively harnessing high-fidelity insight to enhance diagnostic accuracy and agility at scale across the entire patient population.
- Personalization of care models: With rich diagnostic data comes the potential for more personalized interventions, particularly through AI, to discern individualized cardiac indicators among diverse populations. The cardiology clinic of the future believes truly effective care is personalized, and embraces the nuances held in each patient’s heart which hold the secret to better outcomes.
- Virtual-first interventions: The cardiology clinic of the future will redefine traditional boundaries of care, expanding them beyond the clinic’s four walls. With high-acuity diagnostics, strong connectivity and analytical breakthroughs like AI, the virtual cardiology clinic will redefine which portions of care must take place in person. Instead of using virtual care to supplement in-person visits, virtual-first interventions will take shape — transforming the availability of care for patients.
- Unprecedented operational efficiency: The most striking aspect of the clinic is its ability to empower clinicians, utilize data, and personalize care models while also enhancing the efficiency and cost-effectiveness of care. Enhanced preventative measures, streamlined monitoring and increased use of virtual care all enable more efficient care.
But how do we bridge the gap between the cardiology practice of today and the dynamic, future-forward cardiology clinic of tomorrow? At the heart of this metamorphosis are virtual care delivery and AI-enabled virtual cardiac telemetry, which together pave an actionable pathway forward.
The Instrumental Role of Virtual Cardiac Care Delivery and Virtual Cardiac Telemetry
Virtual cardiac care replicates the quality of in-person experiences from nearly anywhere, enhancing continuous and episodic cardiac care. This immediacy in access to clinical support significantly impacts patient outcomes.
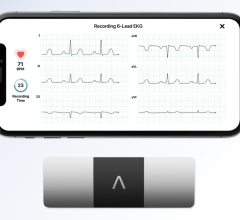
Virtual cardiac care relies on timely cardiac data, which is collected and transmitted through high-acuity virtual cardiac telemetry. As virtual cardiac telemetry becomes more akin to the hospital cardiac monitor in data acuity, new possibilities emerge. For example, during high-risk days post-discharge, complications can be mitigated. One study showed a 23% reduction in hospital readmissions when using remote patient monitoring (RPM).
High-acuity data, while powerful, cannot stand on its own. Large volumes of raw data aren’t digestible or actionable. Fortunately, AI is making its way into both diagnostics and care delivery, with clinical and financial impact. AI adoption in healthcare can save the industry up to $360 billion annually, reducing 86% of errors and potentially saving 250,000+ lives each year.
In cardiology, AI-enabled analytics empower clinicians to transform mass amounts of cardiac monitoring data into tangible takeaways used to enhance diagnostic accuracy and make interventions. In one study, AI enabled multi-class arrhythmia detection with accuracies above 99% in controlled test datasets.
The marriage of virtual cardiac care delivery and virtual cardiac telemetry empowers clinicians to focus their efforts where most needed, enables more timely and accurate diagnoses, and supports the personalization of care models — all with enhanced efficiency. And these technologies are already available. Let’s explore operational tips to adopt virtual care and telemetry effectively, maximizing their value for both practice and patient.
Bringing Technology to Life in Real Clinical Workflows
To support the seamless integration of virtual cardiac care delivery and virtual cardiac telemetry solutions with existing healthcare workflows, practices should take the following steps:
- Conduct a Comprehensive Needs Assessment
One study found that 87% of healthcare organizations have experienced project failure due to the misalignment of technology adoption and organizational requirements, with financial loss estimated at $1.7+ million per incident on average. This underscores the importance of defining requirements at project onset. Practices should evaluate clinical requirements and goals for virtual care delivery and virtual cardiac telemetry, including the most impactful use cases. They should focus on areas where virtual telemetry can improve patient care, security, workflow efficiency, clinician satisfaction, and outcomes.
- Assess Infrastructure Readiness and Ensure Compatibility
An AHA report emphasizes that hospital infrastructure is in dire need of modernization. One challenge is interoperability, with 70% of surveyed hospitals reporting interoperability issues across vendor platforms and systems. Practices should work with IT to ensure virtual telemetry solutions are equipped for easy integration, prioritizing solutions that enable efficient data exchange. In addition, they must ensure their infrastructure supports secure data transmission and storage. Becoming a cardiology clinic of the future means modernizing hardware, software, and networks to accommodate new technologies.
- Start Small and Scale Gradually
It’s important to note that the cardiology clinic of the future isn’t built overnight, nor can transformation be achieved globally and instantaneously. By beginning with a specific clinical use case, practices can identify challenges, validate processes and protocols, and optimize them for scalable success. Metrics for success should be clearly defined from the start (e.g. accelerating time to diagnosis, increasing service line revenue, etc.) Practices should use initial success to build confidence and expand the program gradually across other areas. Twenty percent of large healthcare facilities have already taken this step by adopting some sort of RPM solution for their organization.
- Empower Staff to be Agents of Change
Technology must work for the clinician. Yet 37% of healthcare workers say technology frustrates them, and 19% say it doesn’t help with productivity. The clinical team must buy into the solution and understand how it will help make their lives easier. Practices should provide training programs that demonstrate how to use technology effectively, building confidence in their capabilities and value. Clinical leadership should participate in this charge, educating teams on best practices for interpreting AI-generated data and integrating it into patient care.
- Engage Patients in the Process
Clinicians aren’t the only stakeholders who must be on board. Patient engagement and adherence are key determinants of whether virtual care delivery and virtual cardiac telemetry can realize their intended benefits. Research points to low patient engagement as a predictive indicator of poor outcomes. One report notes less engaged patients are 3x more likely to have unmet medical needs and 2x as likely to delay getting care. Healthcare teams should empower patients with solutions that adhere to best practices for usability, actively evangelize the benefits of adoption and provide tangible tools for ongoing support.
Building the Cardiology Clinic of the Future, Starting Today
Cardiovascular care is undergoing a radical transformation, enabled by groundbreaking technologies. As we stand on the brink of this new era, the opportunity to revolutionize care has never been more essential.
Virtual care delivery and virtual telemetry collectively represent a paradigm shift that promises to enhance diagnostic accuracy, streamline workflows and personalize patient care on an unprecedented scale. Their adoption is crucial to counteracting the rising prevalence of strokes, AFib and other diseases that place immense pressure on already constrained providers. By integrating them into everyday clinical practice, cardiology clinics can transition from reactive care into a proactive, data-driven cardiology clinic of the future.

Stuart Long is CEO of InfoBionic.Ai. He underscores the company’s commitment to widespread market adoption of its transformative wireless remote patient monitoring platform for chronic disease management. With more than 25 years of experience in the medical device market, Long brings expertise in achieving rapid commercial growth. Before joining InfoBionic.Ai, he was CEO at Monarch Medical Systems, LLC, and global chief marketing and sales officer for CapsuleTech, Inc. Long also held executive positions at healthcare IT-focused companies, including Philips Healthcare, Agfa Healthcare, AMICAS, FUJIFILM USA, and Eastman Kodak.

 September 16, 2025
September 16, 2025