Positive AAA Results with Endovascular Approach
Endovascular aortic repair for abdominal aortic aneurysms received a passing grade when compared to traditional open repair. In a review of the first 10 years of use of the endovascular aortic repair at the Jobst Vascular Center, Anthony Comerota, M.D., director of Jobst Vascular Center and adjunct professor of surgery at the University of Michigan, USA, identified 677 patients whom received elective abdominal aortic repair: 427(62 percent) undergoing open surgery and 260 (38 percent) underwent endovascular aortic repair. There were 531 males (78.4 percent) and 146 (21.6 percent) females. An increased number of patients returning home, a decrease in the number of days stayed in the hospital and/or intensive care unit, and lower loss of blood are all factors associated with endovascular aortic repair.
Dr. Comerota said that among the significant difference between the procedures was blood loss. In the open procedure, patients lost an average of 2532 mL of blood, but blood loss was 536 mL with endovascular aortic repair (P<.001 patients="" undergoing="" open="" repair="" spent="" an="" average="" of="" nine="" days="" in="" hospital="" compared="" with="" a="" length="" stay="" for="" endovascular="" aortic="" p="" about="" percent="" who="" underwent="" the="" were="" discharged="" home="" after="" surgery="" to="" had="" repair.="" that="" difference="" also="" achieved="" statistical="" significance="" at="" level="">
Drug Coated Balloons Slow Leg Restenosis
The use of drug-eluting balloon catheters appears to slow restenosis when compared with angioplasty for treatment of blockages in leg arteries.
"Paclitaxel coated balloons could significantly reduce the restenosis rate after angioplasty in the superficial femoral and in the popliteal artery," said Gunnar Tepe, M.D., assistant professor of radiology at the University of Tuebingen, Germany.
In his study of 102 patients who received either standard angioplasty or angioplasty with the balloons coated with paclitaxel, the patients treated with the coated-balloons had significantly less restenosis and less need for repeat procedures. In the primary endpoint of late lumen loss, patients receiving the coated-balloons experienced an average of 0.4 millimeters of lat lumen loss after six months. However, in the patients just given angioplasty, the late lumen loss was 1.7 millimeters with the uncoated balloons. That difference was significant, producing a p<.05 value.="">
Efficacy, Cost-Efficiencies Realized with TEVAR
A review of published literature shows that thoracic endovascular aortic repair (TEVAR) effectively reduces mortality, morbidity, length of stay in the hospital as well as resource utilization.
"The cost of endografts is balanced by reduction in resource utilization and associated costs and justified by improvement in patient outcome," said Dr. Bruce Perler, professor of surgery and chief of the Division of Vascular Surgery at Johns Hopkins School of Medicine, Baltimore.
He predicted that as the endograft repair becomes used more often in more institutions the cost of the devices themselves - estimated to run in the neighborhood of $13,200 -- will be reduced and "will enhance cost efficacy of thoracic endovascular aortic repair."
Perler cited a European study that found the average cost for the thoracic endovascular aortic repair to be about $26,907 - which included the cost of the device. The open surgery averaged around $43,976.
Cutting Balloon Conquers Problems in Angioplasty
The use of the cutting balloon for angioplasty is safe and effective in selected patients - especially those with resistant and recurrent stenotic lesions that often occur in dialysis access.
"Cutting balloon angioplasty may be of specific benefit as primary therapy in situations with a propensity towards restenosis," said David Fox, M.D., chief of vascular surgery at St. Vincent's Midtown Hospital and instructor of clinical surgery at Columbia University College of Physicians and Surgeons in New York.
He said that doctors should apply the cutting balloon can help overcome two problems encountered with angioplasty: (1) Situations where there is a likelihood of a high restenosis rate and (2) A high incidence of balloon resistant lesions — the cutting balloon, estimated to be 3 to 5 times as sharp as a scalpel, creates a lumen that is appears to prevent recoil that sometimes occurs in regular angioplasty.
Dr. Fox suggested that the higher cost of the cutting balloon limits its use to specific treatment circumstances. The estimated cost of the cutting balloon is about $800; a standard angioplasty balloon costs $255. One advantage is that the cutting balloon does not require as much atmospheric pressure to open the stenosed blood vessel. The action of the cutting balloon blades also creates a more regular lumen, whereas the result of the balloon inflation in standard angioplasty creates an irregular lumen that may be prone to clot capture. Dr. Fox said the cutting balloon is also associated with less pain that the standard angioplasty.
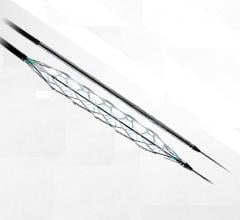
SFA Study Results Compared Stent Placement to Angioplasty Alone
Researchers said they could find no differences in outcomes between femoral arteries opened through angioplasty alone or with angioplasty plus stent placement. "The 'Femoral Artery Stent Trial (FAST)' failed to demonstrate the superiority of the Luminexx nitinol stent of stand alone angioplasty in the treatment of patients with superficial femoral artery lesions 1 to 10 centimeters in length," said Thomas Zeller, M.D., associate professor of vascular medicine at the Heart Center, Bad Krotzingen, Germany.
Although there was no statistically significant difference in overall outcomes, Dr. Zeller did note, "Stent implantation appeared to be associated with a tendency towards a lower risk of restenosis in a wide variety of patients and lesion subgroups."
Dr. Zeller suggested that prospective randomized trial in specific patient cohorts such as diabetics, with total occlusions or patients with impaired distal run-offs are warranted." The goal of the trial was to determine if the Bard Luminexx 3 Vascular Stent or angioplasty produced less binary restenosis at 12 months. After 12 months, in the on-treatment group of patients, binary restenosis occurred in 37.8 percent of patients undergoing angioplasty alone compared with 33 percent of patients who received the Luminexx stent. That difference failed to reach statistical significance (p=.554).
Morbidly Obese Face Ten-Fold Risk of Pulmonary Embolism
Among patients who are morbidly obese - with body mass index of more than 55 - the increasing risk of pulmonary emboli can be reduced virtually 100 percent.
Among the adverse events that can occur during gastric bypass procedures are the risk of blood clots, said Nicholas Gargiulo III, assistant professor of surgery at the Albert Einstein College of Medicine, in The Bronx.
"These patients have a 10 fold risk of having a pulmonary embolism," Dr. Gargiulo said.
He reviewed treatment of obese individuals undergoing gastric bypass surgery since 1999 at his institution, noting that between 1999 and 2001, there were 31 patients who had body mass index over 55 who had the procedure and in 8 of the cases vena cava filters were implanted. Of the remaining 23 patients, four suffered pulmonary emboli, a 17 percent incidence. Between 2001 and 2003, Dr. Gargiulo said 41 of these overweight patients underwent gastric bypass surgery. All of them were protected with vena cava filters and none of them developed pulmonary emboli.
Medical Treatment Preferred for Some AA Dissections
Patients who present with uncomplicated Type B abdominal aorta dissections may be better off receiving conservative treatment rather than undergoing minimally invasive endograft treatment.
"In patients with these types of aortic dissection, the study reveal that a primary strategy of tailored anti-hypertension medical treatment and serial imaging is justified," said Michael Dake, M.D., chairman of the Department of Radiology at the University of Virginia Health System, Charlottesville, "with deferred stent-graft implantation as an option for patients failing to respond to medical management."
In reporting the results of the Investigation of Stent Grafts in Patients with type B Aortic Dissection (INSTEAD), Dr. Dake said the researchers found surprisingly low one year mortality in the medical treatment arm. On the other hand, a slightly higher rate of all cause mortality was seen in the stent graft arm.
There were no deaths among 66 patients who were placed on medical management in the study compared with 7 deaths in 70 patients in the endograft group. Although there were more deaths, in the endograft arm after one year, the difference did not reach statistical significance.
"During the 12-mointh period, 11 percent of the patients assigned to medical management required stent graft implantation," Dr. Dake said. The researchers enrolled 136 patients at 11 European clinical sites in Austria, Germany, France, and Italy. The patients were recruited beginning in 2002 through 2005. Patients had follow-up appointments at 3, 12, and 24 months. The primary end-point for this study was all-cause mortality.
Link Seen Between Carotid Stenting and Cognition
Stenting the carotid arteries of asymptomatic patients with major blockages appears to result in better cognition after one-year.
In an update of data presented at the Society of Interventional Radiology in April 2006 in Toronto, Rodney Raabe, M.D., director of radiology at Sacred Heart Medical Center, Spokane, Wash., said the one-year results not only showed no deterioration in cognitive functioning, but the borderline significant differences from baseline were now more robust.
"The differences in testing scores are now mostly at the p=.001 levels," Dr. Raabe said.
He said that the improvements in scores on several psychological tests continue to be a surprise to him and his fellow researchers. In his study, 62 patients underwent a procedure in which stents were implanted in the carotid arteries of patients who either had strokes, transient ischemic events or had angiography confirming at least an 80 percent occlusion of the artery. Of the 62 patients in the pilot study, 37 have completed one-year follow-up examinations. The patients continue to show improvements on the tests, most scoring even higher than their six month scores. He said 41 patients have completed 6 months since the procedure; 47 have completed three months.
Keynote Cardiologist Explores Heart Disease in Linebackers
During the day Arthur "Archie" Roberts studied the playbook for the Miami Dolphins just in case something happened to starting quarterback Bob Griese. At night he hit medical textbooks, learning how to be a heart doctor. Eventually, Dr. Roberts would prove better at cardiology than football - he played in one game in the National Football League, but rose to be chief of cardiology at Boston University.
Now, retired from the academic world, Roberts has returned to football, trying to find out why the huge athletic men who protected him in the NFL - aka linemen - are more likely to be his heart patients than other players.
In a presentation at the 19th International Symposium on Endovascular Therapy, Roberts, founder of the Living Heart Foundation, Little Silver, N.J., noted, "Large body size is a major risk factor for cardiovascular disease and football players - particularly linemen - are getting bigger and bigger."
The result is the metabolic syndrome: Abdominal obesity, high blood pressure, high blood sugar, high triglycerides and low levels of high-density lipoprotein (HDL) cholesterol - the so-called good cholesterol.
"If you have three of those five conditions, you have the metabolic syndrome which we see as a forerunner of heart disease." During the Super Bowl festivities, Roberts screened 60 former NFL players in a project of his foundation, regional hospitals and the National Football League Players Association. He has already screened more than 900 retired NFL players.
Emergency Docs Saving Patients with Torn Aortas
At McGill University Health Center, the emergency operating room has a cabinet where pairs of endografts are lined up waiting for when that battered but fortunate patient arrives - the one with a torn aorta who despite other traumatic injuries - is still alive when rushed into the hospital. At one point, doctors would have slashed into his chest, split his rib cage and performed a high-risk surgery to repair the torn thoracic aorta.
Since 2002, however, endograft repair has become the emergency procedure of choice for these victims of road accident, falls from high places and unfortunate stumbles in front of trains. The experience at McGill, which is closely monitored by Health Canada, was detailed at the 19th International Symposium on Endovascular therapy.
"We examined our records involving accident patients and no one treated with the endovascular repair has died since we began using it in emergency cases," said Dr. Peter Midgley, a vascular surgeon at McGill, Montreal, Canada. "Most of the people who suffer these injuries never make it to the hospital," Midgley said.
He said 85 percent to 90 percent of these accident victims bleed to death at the scene of the crash - and another 10 percent to 13 percent of these aortic tears rupture once the patient is in the hospital. The average age of the persons in the case series was about 42 years and 20 of the 28 individuals who underwent a procedure were men. The McGill emergency room has handled 30 of these blunt aortic rupture cases since 1994, Midgley said, and until 2002 all were addressed with open surgery - a major operation made even more risky because the patient may have other serious traumatic injuries.
Since 1994, the hospital attempted 16 open surgeries in these blunt trauma patients; five of them died - a mortality rate of more than 30 percent. Another patient was left paralyzed after the life-saving operation. One patient required a re-operation. In two cases the patients' other injuries were too extensive to permit any further treatment. Since 2002, the hospital surgery team has attempted 12 thoracic endovascular aortic repairs - and all the patients survived. None of the patients were paralyzed or required re-operations.

 June 13, 2024
June 13, 2024