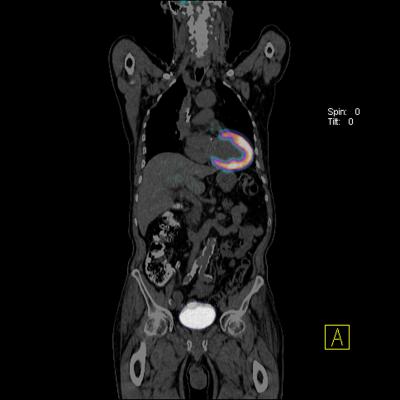
An example of a cardiac PET-CT imaging, should a color coded image of the left ventricle to help assess myocardial perfusion to detect ischemia using a Siemens scanner.
July 19, 2016 - An updated joint American Society of Nuclear Cardiology (ASNC) imaging guidelines and Society of Nuclear Medicine and Molecular Imaging (SNMMI) procedure standard for positron emission tomography (PET) nuclear cardiology procedures has been published in the 2016 September issue of the Journal of Nuclear Cardiology.[1] It addresses the areas of PET myocardial perfusion and metabolism clinical imaging. The new guideline provides imaging guidelines for physicians and technologists who are qualified to practice nuclear cardiology.
Read more on PET vs. SPECT imaging technologies.
The guidelines document is the outcome of close collaboration between SNMMI and ASNC and among experts in the field from both organizations, which has been subjected to extensive review, requiring the approval of several committees from both organizations, and ultimately the endorsement of both SNMMI and ASNC Board of Directors.
To assure quality health care, the Centers for Medicare & Medicaid Services (CMS) has recently implemented quality initiatives that include: effective, safe, efficient, patient-centered, equitable, and timely care. The new guidelines state that the superior imaging properties of PET meet some of the CMS quality goals. Benefits of PET include higher myocardial count density at a shorter image acquisition time than SPECT and less scatter of activity from adjacent sub-diaphragmatic visceral structures into the myocardial region. PET myocardial perfusion imaging provides high diagnostic accuracy (effective), low radiation exposure (safe), short image-acquisition times (efficient), and accommodates ill or higher-risk patients, as well as those with large body habitus (patient-centered), providing equitable and timely care, the guidelines state.
While SPECT assessment of stress and rest myocardial perfusion have been firmly established as important diagnostic and prognostic tools for the evaluation of myocardial ischemia and prior infarction, the interpretation of SPECT myocardial perfusion imaging studies has been primarily qualitative or semi quantitative in nature, the guidelines state. The detrimental effects of soft tissue attenuation, which tends to degrade image quality and increase interpretive errors, have long been recognized with SPECT. The societies consensus is that PET provides better spatial and temporal resolution and allows reliable and accurate soft tissue attenuation correction when compared to SPECT, particularly in patients who are obese or have large body habitus. In concert with tracer-kinetic modeling and robust attenuation correction, PET permits the assessment of regional myocardial blood flow (MBF) of the left ventricle in absolute terms (milliliters per gram per minute).
The guidelines and PET standard article also outlines progress in PET imaging for myocardial perfusion in terms of absolute hyperemic blood flow and flow reserve. Another section explains the progress in PET imaging of glucose metabolism and its use to image cardiac device infections and sarcoidosis.
To access the full article, visit http://link.springer.com/article/10.1007/s12350-016-0522-3
Read an overview of the current PET technology
Recent Advances in Cardiac Nuclear Imaging Technology (Sept. 2017)
Reference:


 January 28, 2026
January 28, 2026 









