
March 5, 2023 — The number of deaths and disabling strokes among patients at low surgical risk who were treated with transcatheter aortic valve replacement (TAVR) remained lower at three years, but not significantly lower, following the TAVR procedure compared with patients who received conventional surgical aortic valve replacement (SAVR), according to new data being presented at the American College of Cardiology’s Annual Scientific Session Together With the World Congress of Cardiology.
In the U.S., the number of people with aortic stenosis who undergo a minimally invasive TAVR procedure now outpaces the number who have conventional valve surgery. However, most of the longerterm data supporting TAVR has come from patients with a higher risk of death or complications from surgery.
“This study shows that the initial benefit of TAVR remained broadly consistent over the first three years,” said John K. Forrest, MD, director of interventional cardiology and structural heart disease at Yale University School of Medicine in New Haven, Connecticut, and lead author of the study. “In patients who are at low risk for death, stroke or other serious complications of aortic valve surgery, we need to have compelling evidence that TAVR is both safe and effective and also that the results are durable. The consistent benefit of TAVR at three years is not something that has been observed in prior studies and provides further evidence that TAVR deserves to be the dominant treatment modality for patients with aortic stenosis undergoing valve replacement.”
The aortic valve connects the heart’s main pumping chamber, the left ventricle, to the body’s main artery, the aorta. Aortic stenosis is a condition that occurs when the aortic valve degenerates, usually due to a buildup of calcium, resulting in restricted blood flow from the left ventricle to the aorta. Symptoms of aortic stenosis may include chest pain, a rapid heartbeat, shortness of breath, dizziness and difficulty walking short distances. Over time, aortic stenosis can lead to heart failure.
TAVR involves using a catheter (a long flexible tube) to place a replacement heart valve inside the patient’s poorly functioning aortic valve, while SAVR involves surgically opening the chest to remove the valve and insert a replacement. The 2020 ACC/American Heart Association Guideline for the Management of Patients With Valvular Heart Disease recommends TAVR over SAVR for patients aged over 80 and SAVR for patients aged under 65 who have a life expectancy of more than 20 years. For patients aged between 65 and 80, the guideline recommends that the choice of TAVR or SAVR be based on shared decision-making by the patient and their cardiologist, Forrest said.
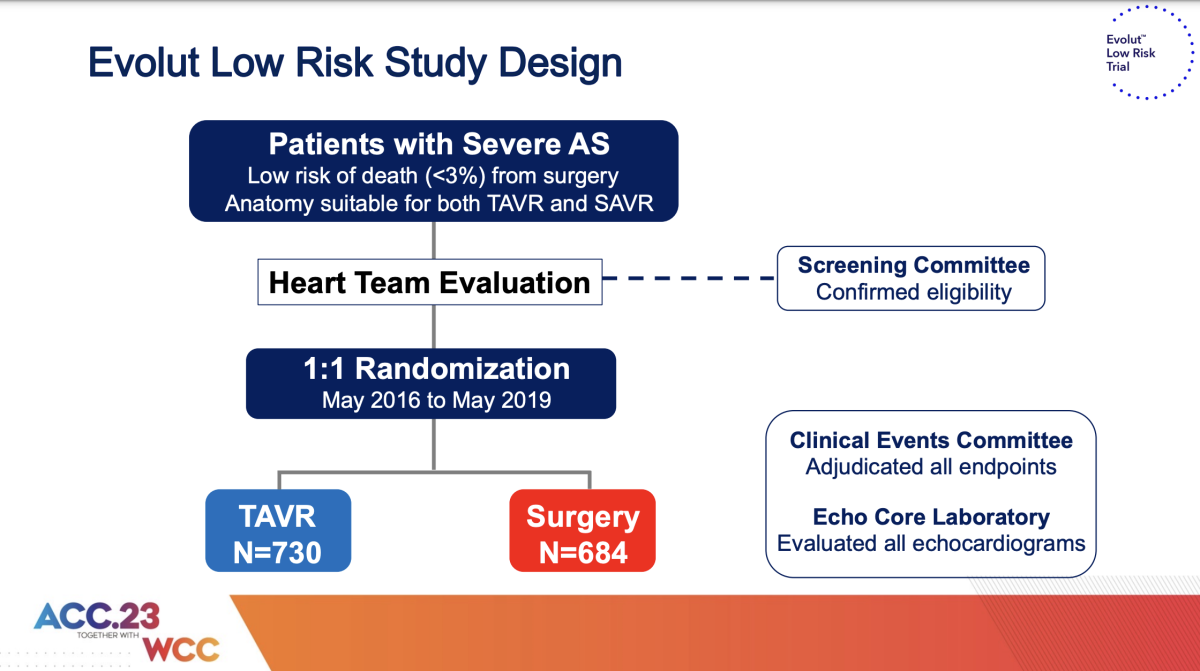
The Evolut Low Risk Trial enrolled a total of 1,468 patients in seven countries (Australia, Canada, France, Japan, the Netherlands, New Zealand and the U.S.), of whom the median age was 74 years and 35% were women. All had severe symptomatic aortic stenosis and were deemed to be at low risk from surgery, defined as having no more than a predicted 3% risk of death within 30 days of the procedure. Half of the patients were randomly assigned to receive TAVR and half to SAVR.
The study’s primary endpoint was a combination of death from any cause or a disabling stroke at two years. Secondary endpoints included death from any cause, a disabling stroke or readmission to the hospital for an aortic valve blockage; the percentage of patients experiencing leakage of blood around the replacement valve or needing a permanent new heart pacemaker; and improvement in patients’ quality of life.
A prespecified interim analysis, conducted after a median follow-up period of 12.2 months and published in the New England Journal of Medicine in May 2019, estimated statistically that 5.3% of patients in the TAVR group would experience the primary endpoint within 24 months, compared with 6.7% in the SAVR group, suggesting that TAVR was “noninferior” to SAVR at two years.
In the current study, after all patients had been followed for at least three years, 7.4% of those treated with TAVR had died or had a disabling stroke, compared with 10.4% of those treated with SAVR, a difference that fell just short of statistical significance. Occurrence of the secondary combined endpoint of death from any cause, a disabling stroke or readmission to the hospital for an aortic valve blockage was significantly lower for the TAVR group (13.2%) than the SAVR group (16.8%).
More patients in the TAVR group than the SAVR group experienced mild leakage of blood around the replacement heart valve (20.3% vs. 2.5%); however, this finding was not associated with an increase in deaths or disabling stroke. In addition, compared with SAVR patients, more TAVR patients needed permanent new heart pacemakers (9.1% vs. 23.2%).
In both groups, about 1% of patients needed a repeat aortic valve replacement procedure and less than 1% experienced a blood clot on the replacement valve. At 30 days after their procedure, TAVR patients reported greater improvement in quality of life compared with SAVR patients; however, at three years both groups reported similar improvements in quality of life.
In addition to being deemed low risk for death or a stroke following surgery, patients enrolled in the study were also required to have “favorable anatomy” for TAVR, Forrest said—for example, patients with large, bulky calcium deposits in the aortic valve or other disease features that increased the likelihood of TAVR failure were excluded from the study.
Since the Evolut Low Risk Trial was completed, the replacement valves it used have been replaced by a new generation of devices that have been shown to reduce leakage of blood around the replacement valve, Forrest said. A higher incidence of new pacemaker placement remains a risk for TAVR patients receiving certain types of replacement aortic valves, he said.
While the current study’s findings are largely reassuring, Forrest said, longer-term data for low-risk patients are still needed and patients enrolled in the study will be followed for 10 years. “Patients with severe aortic stenosis who are at low surgical risk should continue to engage in shared decision-making with their physicians concerning the risks and benefits of surgical versus transcatheter valve replacement,” Forrest said.
The study was funded by Medtronic, manufacturer of the aortic valve replacement devices used in the trial.
This study was simultaneously published online in the Journal of the American College of Cardiology at the time of presentation.
For more information: www.acc.org


 July 31, 2024
July 31, 2024 









