November 7, 2016 — Keystone Heart Ltd. announced that data presented at the Transcatheter Cardiovascular Therapeutics (TCT) 2016 scientific symposium demonstrate an increase in brain lesions for patients following transcatheter aortic valve replacement (TAVR) procedures, which were significantly associated with delirium.
"It is imperative that we take steps toward preventing damage to the brain during TAVR," said Peter R. Stella, M.D., Ph.D., Department of Cardiology, University Medical Centre Utrecht, Utrecht, The Netherlands, who led the study. "These results clearly demonstrate that the quality of life for patients undergoing TAVR can deteriorate substantially if the brain is not protected, and to date the guidelines do not suggest that we need to take any precautions."
Watch the VIDEO “Defining the Need for TAVR Embolic Protection.”
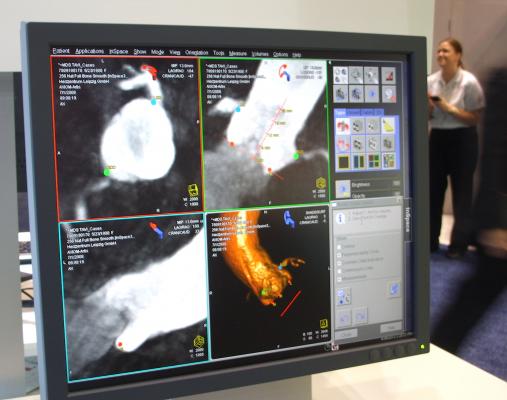
In the study, 90 percent of patients (n=103) undergoing TAVR demonstrated lesions in the brain following TAVR procedure, based on evaluation using diffusion weighted magnetic resonance imaging (DW-MRI). Of these, 14.5 percent (n=15) were identified as having post-operative delirium (POD) using the Delirium Observational Scale based on Diagnostic and Statistical Manual of Mental Disorder, 4th Edition criteria.
The number of new cerebral DWI-lesions was higher in patients with POD (8[5-15] vs.4 [2-7], p=0.023). After controlling for several confounding factors (e.g., global cortical atrophy, white matter abnormalities, logistic EuroSCORE, access site), the number of DWI-lesions significantly associated with POD remained higher (Odds Ratio 1.08; 95 percent confidence interval 1.10-1.16, per number of DWI-lesions increase).
Post-op delirium in TAVR patients has been shown to lead to a three-fold increase in both post-procedural and long-term mortality, according to previously published data (Giuseffi JL, J Am Coll Cardiol. 2014;63:12, Abawi M, J Am Coll Cardiol Intv. 2016;9:160.) Other studies have also shown that post-op delirium can lead to extended length of stay and in-hospital complications, as well as an increase in healthcare costs of between $16,000 to $64,000 per patient (Leslie DL, J Am Geriatr Soc. 2011;59:S241).
Numerous other studies conducted in Europe laid the groundwork for these findings, with their data demonstrating that 58-100 percent of patients have new brain lesions following TAVR. The recently published NeuroTAVR study, conducted out of Yale, shows that 94 percent of patients (n=44) had new lesions in the brain following the TAVR procedure, 22.6 percent of patients had new neurologic impairment post-TAVR, and 41 percent of patients had declining neurocognition at 30 days when compared to pre-TAVR scores in the United States.
Data presented as part of PCR London Valves 2016 by Alexandra J. Lansky, M.D., Division of Cardiology, Yale School of Medicine and Yale Cardiovascular Research Group, New Haven, Conn., demonstrated the safety and efficacy of the TriGuard Cerebral Embolic Protection device when used during TAVR. Use of the device, which provides protection for all three arteries that provide blood flow to the brain, showed significant reduction of all stroke and neurologic decline. According to preliminary findings from this real-world experience from University Medical Centre Utrecht, Utrecht, The Netherlands and Hamburg University Cardiovascular Center and Department of Structural Heart Disease, Hamburg, Germany, no patients had strokes with TriGuard protection and in a subgroup of patients with DW-MRI, only 20 percent of patients had new lesions compared to close to 70 percent of patients without embolic protection.
Read the article, “TAVR Embolic Protection Did Not Reduce Emboli Brain Lesions.” This is for a second trial presented at TCT for a TAVR embolic protection system, but data was not that positive for the Claret Medical’s Sentinel transcatheter cerebral embolic protection system.
For more information: www.crf.org/tct


 November 14, 2025
November 14, 2025 









