April 1, 2008 — An angioplasty balloon coated with a drug that reduces renarrowing of the coronary arteries appears to be more effective than a drug-eluting stent in treating an unwanted build-up of tissue inside a bare-metal coronary stent. After six months, the newly expanded artery remained more widely open within the stent after treatment with the paclitaxel-eluting balloon when compared to a paclitaxel-eluting stent, according to the Paclitaxel-Eluting PTCA-Balloon Catheter in Coronary Artery Disease II-In-Stent Restenosis (PEPCAD II-ISR) study. Additional data suggested that at one year, rates of major cardiac events were also lower with the drug-coated balloon.
The PEPCAD II-ISR study was reported yesterday at the SCAI Annual Scientific Sessions in Partnership with ACC i2 Summit (SCAI-ACCi2) in Chicago. SCAI-ACCi2 is a scientific meeting for practicing cardiovascular interventionalists sponsored by the Society for Cardiovascular Angiography and Interventions (SCAI) in partnership with the American College of Cardiology (ACC).
“This drug-eluting balloon clearly qualifies for consideration as an alternative to drug-eluting stents for the treatment of restenosis inside bare-metal stents,” said Martin Unverdorben, M.D, Ph.D, an associate professor of medicine at the University of Frankfurt/Main, Germany. “However, two to three years’ more data are required before making a definitive statement.”
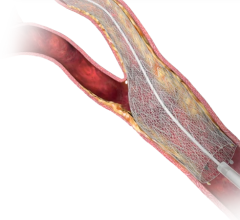
In-stent restenosis remains a challenge, despite the availability of drug-eluting stents. Approximately 25 percent of patients treated with a bare-metal stent and about 10 percent of patients treated with a drug- eluting stent develop an overgrowth of vascular tissue and renarrowing inside the stent, or in-stent restenosis.
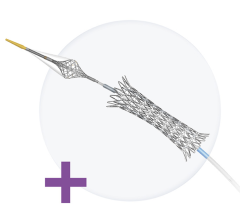
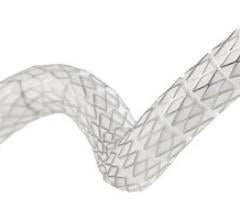
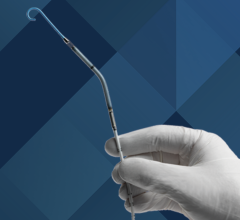
Treating in-stent restenosis with a drug-eluting stent is a complex procedure that adds another layer of metal to the artery and can create mechanical problems. The Sequent Please drug-eluting balloon may offer a simpler alternative. This drug-eluting balloon is coated with paclitaxel, the same medication that coats the Taxus stent. The balloon is inflated for about 30 seconds inside the narrowed artery, and the paclitaxel—which has a natural attraction to cells—quickly moves from the surface of the balloon into the arterial cells.
Not only does the drug-eluting balloon avoid a second layer of metal inside the artery, the carrier that is used to bind paclitaxel to the balloon is iopromide, a commonly used contrast agent. This avoids concerns about the artery’s reaction to the polymers used to bind paclitaxel and other anti-restenosis medications to drug-eluting stents.
The study was conducted at the Center for Cardiovascular Diseases in Rotenburg an der Fulda, Germany. Dr. Unverdorben and his colleagues recruited 131 patients with restenosis in a bare-metal stent, randomly assigning them to treatment with the Sequent Please drug-eluting balloon (DEB) or the Taxus drug-eluting stent (DES). Five patients were excluded for protocol violations, and four patients in the stent group were actually treated with the drug-eluting balloon. This left, for the “as- treated” analysis, 66 patients in the DEB group and 60 patients in the DES group.
The researchers initially analyzed the data according to each patient’s original treatment assignment (the intention-to-treat analysis). After an average of six months of follow-up, late-lumen loss—the amount of tissue that grew from the vessel wall into the arterial lumen—was significantly less in the patients treated with the DEB (0.20 mm vs. 0.45 mm, p=0.02). When the data were analyzed according the treatment each patient actually received, the results were even more promising. Late-lumen loss remained significantly better with the drug-eluting balloon. In addition, a finding of significant renarrowing in the treated segment was less common in the DEB group (3.4 percent vs. 20.4 percent, p=0.007), as was the need for a repeat procedure to re-treat the target lesion (3.1 percent vs. 16.7 percent, p=0.02). Combined rates of major cardiovascular events, defined as heart attack, repeat procedure to treat the target lesion and cardiac death were 4.7 percent and 18.3 percent, respectively (p=0.02).
Between six and 12 months, two patients in the DEB group needed PCI in another artery, and one patient (1.5 percent) needed yet another PCI to treat the original target lesion. In the DES group, two patients died of noncardiac causes, and three patients (5 percent) needed repeat target-lesion PCI. No new patients experienced a major cardiac event.
At 12 months, there was a trend toward better event-free survival in patients treated with the DEB in the intention-to-treat analysis. The difference was statistically significant (p=0.01) when the analysis was done according to the as-treated analysis.
For more information: www.scai-acci2.org

 November 24, 2025
November 24, 2025