September 18, 2019 — Early use of an implantable cardioverter-defibrillator (ICD) after primary coronary intervention lengthens survival in patients at high risk of death after ST-segment elevation myocardial infarction (STEMI). The late-breaking results from the DAPA trial were presented in a Hot Line Session at the European Society of Cardiology (ESC) Congress 2019, Aug. 31-Sept. 4 in Paris, France, together with the World Congress of Cardiology.
First author Danielle Haanschoten, M.D., of Isala Hospital, Zwolle, the Netherlands said, “The results of the DAPA trial indicate that certain high-risk patients may benefit from early ICD implantation after primary percutaneous coronary intervention (PCI). However, the study was stopped prematurely. Therefore, more research is needed to support these findings.”
ESC guidelines recommend prophylactic ICD implantation at least six weeks after myocardial infarction in ischaemic etiology. [1] American guidelines recommend prophylactic ICD implantation at least 40 days after myocardial infarction and at least 90 days after revascularization.[2]
Haanschoten said, “Advice to delay ICD use is based on the fact that implantation within 40 days was not studied in MADIT II and SCD-HeFT and did not show a survival benefit in two primary prevention trials (DINAMIT and IRIS). It has been unclear which patients might gain from a prophylactic ICD to reduce sudden cardiac death after primary PCI.”
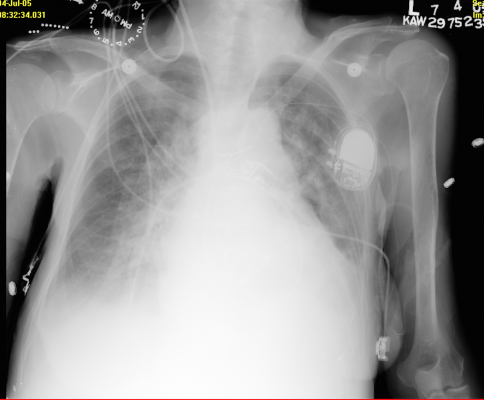
The aim of the DAPA trial was to examine whether ICD implantation between 30 and 60 days after primary angioplasty for STEMI would provide a survival benefit in patients at high risk of death.[3] High risk was defined as at least one of the following: primary ventricular fibrillation, left ventricular ejection fraction below 30 percent, Killip class 2 or higher, or TIMI flow less than 3 after primary PCI.
Patients were randomly allocated to prophylactic ICD implantation or optimal medical therapy. The primary endpoint was all-cause mortality after at least three years of follow-up for each patient. Secondary endpoints were cardiac death and sudden cardiac death.
The trial was halted prematurely in 2013 on advice of the data safety monitoring board due to a slow inclusion rate. A total of 266 patients were randomized and followed-up for a median of nine years.
ICD implantation significantly lowered the risk of all-cause and cardiac mortality. All-cause mortality occurred in 24.4 percent of the ICD group versus 35.5 percent in the control group, with a hazard ratio (HR) of 0.58 (95 percent confidence interval [CI] 0.37–0.91). The rate of cardiac death was 11.4 percent in the ICD group and 18.5 percent in the control group (HR 0.52; 95 percent CI 0.28–0.99). Rates of sudden cardiac death were not significantly different between groups.
Haanschoten said, “The all-cause mortality curves started to diverge before the first year and the beneficial effects of prophylactic ICD use were preserved throughout the nine-year follow-up. The survival advantage of ICD implantation was mainly driven by a reduction in cardiac mortality.”
She concluded, “Together with results of previous trials, the DAPA trial may contribute to early selection of high-risk patients who will profit from an ICD after primary PCI for STEMI. The unexpected ending of the study is an important limitation and further studies are needed before any change in practice can be considered.”
For more information: www.escardio.org
References
1. Priori S.G., Blomström-Lundqvist C., Mazzanti A., et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2015;36:2793–2867. doi:10.1093/eurheartj/ehv316.
2. Al-Khatib S.M., Stevenson W.G., Ackerman M.J., et al. 2017 AHA/ACC/HRS Guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. J Am Coll Cardiol. 2018;72:e91–e220. doi: 10.1016/j.jacc.2017.10.054.
3. Ottervanger J.P., Ramdat Misier A.R., Zijlstra F., et al. Implantable defibrillator early after primary percutaneous intervention for ST-elevation myocardial infarction: rationale and design of the Defibrillator After Primary Angioplasty (DAPA) trial. Am Heart J. 2006;152:636–640.


 January 05, 2026
January 05, 2026 









