Indiana University (IU) Health La Porte Hospital in La Porte, Ind., worked with GE Healthcare to create a state-of-the-art arrhythmia center to help reduce the number of electrophysiology referrals to hospitals in Chicago.
Indiana University (IU) Health La Porte Hospital in La Porte, Ind., is a full-service, 227-bed, acute care, non-profit hospital serving the local community as well as Northwest Indiana. The hospital spent almost three years operating from a modular electrophysiology (EP) lab, performing more than 800 procedures. During that time, it was mostly limited to simple ablations and device implants. The need for a local EP lab with advanced technology was evident, but the staff was also looking to increase the hospital’s efficiency and improve hospital processes at the same time. La Porte not only needed a procedure lab, but also space for admission and recovery of the patients, and was looking to reduce the need for an in-house nursing unit that could affect turnaround times and delay procedures.
The Challenge
La Porte is a small community located in the shadow of Chicago. Patients can get to downtown Chicago in about one hour, so without an aggressive EP program at the facility, patients were often transferred to university centers in Chicago. This was difficult for the patients, particularly the elderly, who were unfamiliar with where to go and how to get there. The La Porte community is agriculture- and industry-based, consisting of tight-knit residents who support the local hospital and want to be treated there rather than go to other locations for their care. Sending patients elsewhere also put the hospital at an economic disadvantage.
“Patients were often transferred out in an acute state to one of the other facilities,” said Chris Atherton, RN, BSN, MPA, director, Arrhythmia Center. “We felt it was important to offer the services here not only to perform the procedural services, but also have a clinic that’s associated with the hospital.”
The Solution
The hospital made the decision to build an advanced EP procedure lab right in the community with holding areas, ancillary workspaces, office space and a clinical area. The vision was for the lab to encompass all aspects of arrhythmia care, beginning at the procedure area and finishing with the outpatient clinic. It also was extremely important that the space was efficient, cost-effective and flexible.
The 6,100-square-foot lab was completed in three phases. Phase 1 included a dedicated EP lab/control room – a holding room with patient monitors connected to a central nursing station and the patient data. Phase 2 included a second lab and control room that would be utilized for electrophysiology cases as well as interventional cardiology procedures, two more holding rooms, clean and dirty utility rooms, a staff dressing room and bathrooms. Phase 3 was dedicated to the clinic and included three clinic rooms, a nurses’ station, a staff lounge, a family waiting room, a consultation room as well as offices for the medical director, nursing director and trans-telephonic pacing personnel.
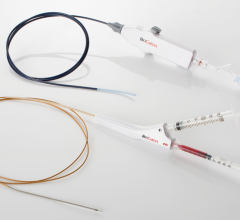
From the beginning, the team knew what equipment was required in the lab – biplane fluoroscopy with rotational angiography, 3-D mapping and an intra-cardiac echo (ICE) system in addition to an EP recording system. Careful evaluation of the technology helped ensure that the new system could be paperless and the elements would work together to help improve workflow.
With efficiency as a top priority, keeping the rooms free of the cables that are associated with complex EP procedures was a necessity. Anesthesia was integrated into the equipment management boom with fittings for applicable gas utilization. For the recording system, it was essential that the nursing staff documented all care in one system, from the time the patient entered the holding area, throughout the procedure, until discharge. This made remote workstations a key consideration.
After researching different equipment companies, IU Health La Porte Hospital carefully evaluated how each product would meet its needs. The team decided that it would purchase fluoroscopy equipment, an EP recording system, DASH patient monitors with central station monitoring and an interventional ultrasound system from GE Healthcare. STERIS Corp. would provide surgical lighting, anesthesia and equipment booms. Biosense Webster Inc. was utilized for 3-D mapping. Hansen Medical also provided a robotic system.
Because the majority of the equipment was purchased through GE, IU Health La Porte Hospital was given a project manager to coordinate the efforts of all of the vendors and divisions. They coordinated the services from GE and also worked with representatives from Biosense Webster and Hansen Medical to troubleshoot issues.
“One of the most important aspects of this process was the project management team I worked with from GE,” said Atherton. “I was really involved with the construction, but I was able to have the assistance of the project manager, who also acted as my contractor.”
Benefits of the New Lab
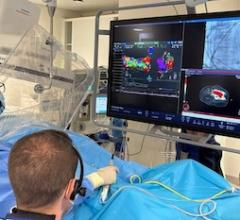
IU Health La Porte Hospital is now a full-service lab. With the integration of the 3-D mapping technology and echocardiography, they can perform complex ablations and have increased the amount of ablations that are performed.
The lab was designed to have optimal imaging quality to facilitate performing complex catheter ablation procedures and GE Healthcare’s fluoroscopic equipment has been invaluable in imaging the hearts in a variety of ways to facilitate these procedures.
The cath lab uses GE’s Mac-Lab Hemodynamic Recording System and the EP lab uses the CardioLab EP Recording System. Admission, discharge and transfer (ADT) information and procedural results are exchanged quickly and easily between hospital systems, because they are networked within the hospital. The team is comfortable with the new technology because they found it easy to use.
It was also evident from the beginning that, with this technology, the new lab staff could accurately monitor the total irradiation time of the patient with the exam. “During the first three days of the clinical applications, the clinical instructor would tell us to look at our fluoro time,” said Atherton. “We were performing some very complex cases with excellent images using low-dose levels.”
According to Atherton, the new EP lab has enabled excellent outcomes and efficiency and gives them the ability to offer advanced EP technology right in their own community, which is extremely important to the staff conducting the procedures and the patients receiving the care.
“The technology, as it has expanded, has enabled us to do more in less time,” said Mark Dixon, D.O., medical director of the Arrhythmia Center. “For example, atrial fibrillation or ventricular tachycardia ablations are two of the most demanding procedures that we do. They are hard on the staff and can be very rigorous on the patient. With the technology we have in this lab, I am able to reduce these procedure times. Our success rates for these complex ablations have gone up significantly from the days when we were first trying to do them by hand, in what I call the so-called primitive days of electrophysiology.”
This case study was supplied by GE Healthcare.


 January 29, 2026
January 29, 2026