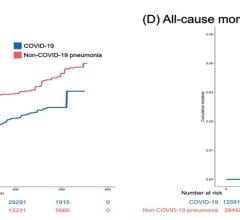
A new study with data from more than 10,000 COVID patients confirmed that patients taking statin medications had a 41 percent lower risk of in-hospital death from COVID-19. Researchers believe statins, which attach to the ACE2 receptors, may block the virus from attaching to these same receptors.
July 21, 2021 — In a new study from University of California San Diego School of Medicine, researchers have confirmed that patients taking statin medications had a 41 percent lower risk of in-hospital death from COVID-19. The findings were published July 15, 2021 in Plos One and expand upon prior research conducted at UC San Diego Health in 2020.[1]
Statins are commonly used to reduce blood cholesterol levels by blocking liver enzymes responsible for making cholesterol. They are widely prescribed, with the Centers for Disease Control estimates that 93 percent of patients who use a cholesterol-lowering drug use a statin.
“When faced with this virus at the beginning of the pandemic, there was a lot of speculation surrounding certain medications that affect the body’s ACE2 receptor, including statins, and whether they may influence COVID-19 risk,” said Lori Daniels, M.D., lead study author, professor and director of the Cardiovascular Intensive Care Unit at UC San Diego Health. “At the time, we thought that statins may inhibit SARS-CoV-2 infection through their known anti-inflammatory effects and binding capabilities, which could potentially stop progression of the virus.”
Using data from the American Heart Association’s COVID-19 Cardiovascular Disease Registry, the research team at UC San Diego applied their original findings to a much larger cohort — more than 10,000 hospitalized COVID-19 patients across the United States.
Specifically, researchers analyzed anonymized medical records of 10,541 patients admitted for COVID-19 over a nine-month period, January through September 2020, at 104 different hospitals.
“From this data, we performed more advanced analyses as we attempted to control for coexisting medical conditions, socioeconomic status and hospital factors,” said Daniels. “In doing so, we confirmed our prior findings that statins are associated with a reduced risk of death from COVID-19 among patients hospitalized for COVID-19.”
Daniels said it appears most of the benefit is among patients with good medical reasons to be taking statins, such as a history of cardiovascular disease or high blood pressure. According to the research team, the use of statins or an anti-hypertension medication was associated with a 32 percent lower risk of death among COVID-19 inpatients with a history of cardiovascular disease or hypertension.
In the study, statistical matching techniques were used to compare outcomes for patients who used statins or an anti-hypertension medication with similar patients who did not.
“We matched each patient to one or more similar patients, using hospital site, month of admission, age, race, ethnicity, gender, and a list of pre-existing conditions, in order to make the two groups as comparable as possible” said Karen Messer, Ph.D., study co-author and professor of biostatistics at UC San Diego School of Medicine.
The ACE2 receptor — the regulatory target of statins — helps control blood pressure. In 2020, it was discovered that SARS-CoV-2 virus primarily uses the same receptor to enter lung cells.
According to researchers, statins and anti-hypertension medications stabilize the underlying diseases for which they are prescribed, making patients more likely to recover from COVID-19.
“As with any observational study, we cannot say for certain that the associations we describe between statin use and reduced severity of COVID-19 infection are definitely due to the statins themselves; however, we can now say with very strong evidence that they may play a role in substantially lowering a patient’s risk of death from COVID-19,” explained Daniels. “We hope that our research findings are an incentive for patients to continue with their medication.”
The initial study included 170 anonymized medical records from patients receiving care at UC San Diego Health. Researchers found that statin use prior to hospital admission for COVID-19 resulted in a more than 50 percent reduction in risk of developing severe infection.
The American Heart Association’s COVID-19 Cardiovascular Disease Registry contains de-identified health data on patients treated for COVID-19 at more than 140 participating hospitals across the country. As of July 2021, data from more than 49,000 patient records had been contributed into the platform.
Co-authors of the study include: Junting Ren, Quan M. Bui, Jing Zhang, Xinlian Zhang, Christopher A. Longhurst, all at UC San Diego; Kris Kumar, Knight Cardiovascular Institute; Mariem A. Sawan, Emory University School of Medicine; and Howard Eisen, Pennsylvania State Health.
No funding was reported for this study.
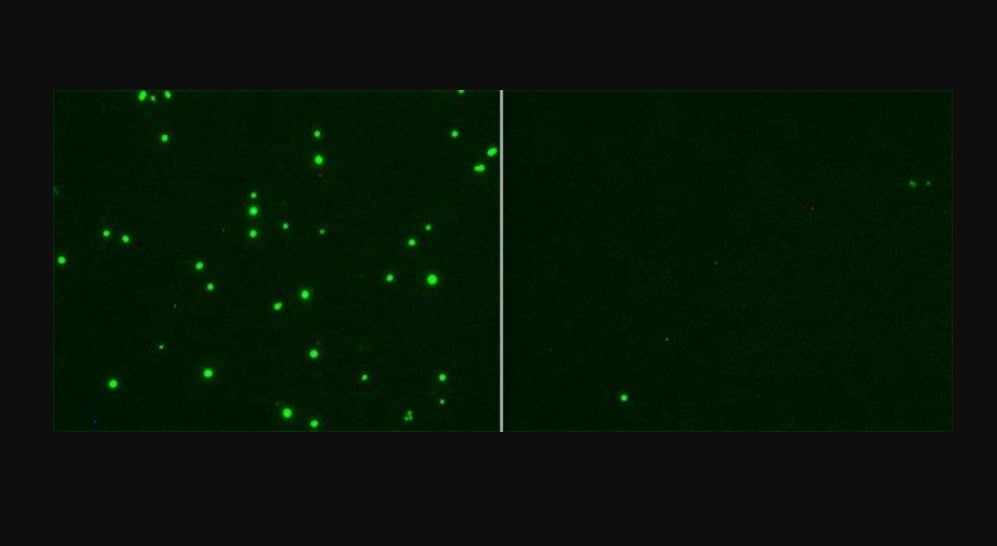
SARS-CoV-2 infection of cells shown in green, left. This is inhibited by a modified form of cholesterol called 25-hydroxycholesterol (25HC), as seen in the cells in the right image. 25HC activates an enzyme called ACAT, found inside cells in the endoplasmic reticulum. ACAT then depletes accessible cholesterol on the cell’s membrane. It is a normally occurring process that gets kicked into high gear during some viral infections. Image from UC San Diego Health Sciences.
Related ACE Content Related to COVID-19:
Statins May Reduce COVID-19 Severity (initial UCSD 2020 study)
ESC Council on Hypertension Says ACE-I and ARBs Do Not Increase COVID-19 Mortality
First Randomized Trial Backs Safety of ACE and ARB Heart Drugs in COVID-19 Patients
No Evidence Supporting Discontinuing RAAS Inhibitors in COVID-19 Patients
References:

 March 20, 2024
March 20, 2024