October 3, 2011 – Researchers from MIT’s Computer Science and Artificial Intelligence Laboratory (CSAIL), the University of Michigan, Brigham and Women’s Hospital in Boston and Harvard Medical School have developed a new tool that can more accurately determine risk of death in patients who have suffered a heart attack. Results of the study could prove life saving for the millions of Americans who suffer heart attacks every year.
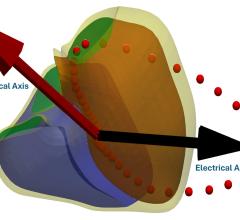
The new technique involves searching for subtle indicators of risk hidden in a patient’s electrocardiogram (ECG) history. The electrocardiogram measures and displays the electrical activity of the heart. Current techniques for determining risk of death in patients who have suffered a heart attack tend to only identify a small portion of resulting fatalities.
The study was conducted by MIT EECS professors and CSAIL principal investigators John Guttag and Collin Stultz (who is also an investigator in MIT RLE), University of Michigan professor (and MIT EECS and CSAIL alumnus) Zeeshan Syed and Brigham and Women’s Hospital cardiologist Benjamin M. Scirica. Results of the study are published in a new paper in the Sept. 28 edition of Science Transitional Medicine.
Researchers developed three new risk factors that can be identified by employing computer science techniques to sift through hours of a patient’s ECG recordings, a task that is too time-consuming for doctors and nurses.
“The basic idea is that there are a lot of interesting phenomena that are hard to observe looking at little snippets of data, but that are visible when you look at large chunks of data,” explained Guttag. “It lets you sift through massive amounts of data and draw conclusions.”
Researchers examined how using these new indicators might be combined with current methods for determining risk in particular echocardiograms and the TIMI risk score, which is based on a patient’s medical history. While both of these techniques provide useful information, researchers were looking to develop a new method to enhance current risk assessment strategies.
“Today’s methods for determining which heart attack victims need the most aggressive treatments can identify some groups of patients at a high risk of complications. But they miss most of the deaths –– up to 70 percent of them,” said Syed, an assistant professor in the University of Michigan Department of Electrical Engineering and Computer Science and first author of the study.
Using data mining and machine-learning techniques, the researchers sifted through 24-hour continuous ECGs from 4,557 heart attack patients enrolled in a large clinical trial led by the Brigham and Women’s Hospital/Harvard Medical School TIMI Study Group, one of the world’s leading cardiovascular research organizations.
Based upon a belief that current risk assessment techniques miss potentially important information, researchers invented three new metrics, called computational biomarkers, for determining risk of death. The biomarkers (morphologic variability, heart rate motifs and symbolic mismatch) signal heart defects and abnormalities that occur repeatedly over long periods of time, information often overlooked during routine examination of a patient’s ECG recordings, which typically focus on much smaller segments of data.
Morphologic variability measures the electrical stability of the heart, a potential clue in identifying heart attack risk. Heart rate motifs looks for heart rate patterns that could be indicate heart problems. Symbolic mismatch compares ECG histories of sick and healthy patients for similarities and differences that could help determine the health of the heart.
Results of the study showed a strong correlation between the three biomarkers and cardiovascular death over the two-year period following a heart attack. For example, they found that those with at least one of the abnormalities were between two and three times more likely to die within 12 months of having a heart attack. By adding all three of the techniques to doctors’ current assessment tools, they could predict 50 percent more deaths with fewer false positives than when predictions were made based upon data retrieved from echocardiograms.
An important aspect of this study is that it could be implemented into current medical practices without imposing any additional burden or cost. Information required to identify the three biomarkers is already gathered through ECG monitoring conducted during routine examinations of patients who have suffered heart attacks.
“It doesn’t require acquiring any data that’s not already routinely acquired. It imposes no extra labor, no extra financial burden, it just takes data that they gather anyway and analyzes it in a different way,” said Guttag. “Therefore, it’s a lot easier to envision how it could get done than if you’d asked them to perform some tests that they don’t routinely perform. It’s not adding any burden to the caregivers or to the patient.”
Using the biomarkers not only improved patient risk classification, but researchers also hope it will prove helpful in selecting treatment methods for patients following a heart attack.
Going forward, researchers hope to apply their work with biomarkers to other areas of medicine where data mining and machine learning techniques could be used to help sort through large amounts of information for clinically useful indicators.
“Our findings demonstrate that low-cost, non-invasive and easily obtained biometric data, such as the ECG, can be used to identify patients at high risk of adverse outcomes. We hope that this work ignites a new paradigm in the field of cardiovascular risk stratification,” said Stultz.
This research was funded by the National Science Foundation, the Center for Integration of Medicine and Innovative Technology, Quanta Computer, and the Harvard-MIT Division of Health Sciences and Technology. The paper is titled “Computationally Generated Cardiac Biomarkers for Risk Stratification Following After Acute Coronary Syndrome.” Ongoing research is supported by the American Heart Association.


 January 15, 2026
January 15, 2026