January 31, 2012 — Updated appropriate use criteria offer detailed guidance on when to use an invasive procedure to improve blood flow to the heart and how to choose the best procedure for each patient. The clinical scenarios, written by a group of cardiologists and cardiac surgeons, affirm the role of revascularization for patients with acute coronary syndromes and significant symptoms.
“This document helps patients, physicians and payers determine when it’s reasonable to do a procedure that is intended to improve the patient’s quality of life, health status and long-term survival,” said Manesh Patel, M.D., the John Bush Simpson assistant professor of cardiology at Duke University in Durham, N.C., and lead author of the updated appropriate use criteria. “It can also assist patients and physicians with health-related discussions and shared decision-making, so that patients are confident they are getting the right procedures for them.”
The criteria replace a previous set published in 2009. Both documents were jointly developed by the American College of Cardiology Foundation, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America and Society of Cardiovascular Computed Tomography. They have been endorsed by the American Society of Echocardiography and Heart Rhythm Society.
When developing the 2009 appropriate use criteria, the writing group identified nearly 200 clinical scenarios that reflect common heart problems seen in everyday cardiology practice. These scenarios were rated by an expert panel composed of interventional cardiologists, heart surgeons, non-interventional cardiologists, other physicians who treat patients with cardiovascular disease, health outcomes researchers and a medical officer from a health plan. Panelists assigned a score using a modified Delphi exercise to each scenario indicating whether an invasive procedure to restore blood flow to the heart would be considered appropriate, inappropriate or uncertain. An essential component in evaluating each clinical scenario is whether clinical studies have shown the procedure would be likely to improve patients’ survival or quality of life. The rating takes into account such factors as symptoms, medication, results of stress testing, severity of disease, burden and number of coronary blockages.
New clinical data and gaps identified in data collection spurred the update of the appropriate use criteria, Patel said. “This update provides a reassessment of clinical scenarios the writing group believed to be affected by significant changes in the medical literature or gaps from prior criteria,” he said. “For example, publication of the SYNTAX trial called for the reexamination of clinical scenarios for multi-vessel coronary artery disease, and implementation efforts revealed a few scenarios not captured in the 2009 publication.”
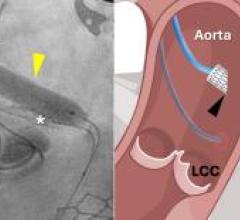
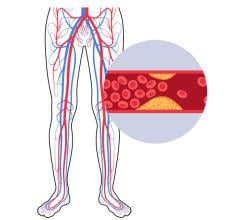
When a patient’s coronary arteries become clogged with deposits of cholesterol and fat, the heart muscle may not get enough blood flow to function properly. The result can be chest pain or even a heart attack. If medication and lifestyle changes alone are not enough, physicians and patients must decide whether to improve blood flow with bypass surgery or catheter-based angioplasty and stenting. That decision is based not only on a patient’s overall health and personal preferences, but also on which arteries are clogged and how severely.
Symptom status, extent of medical therapy, risk level as assessed by noninvasive testing and coronary anatomy all play a critical role in decision making. The appropriate use criteria scenarios were developed to mimic patient presentations encountered in everyday practice and to address the rational use of coronary revascularization in the delivery of high-quality care. Appropriate revascularization procedures can improve patients’ clinical outcomes, whereas inappropriate revascularization exposes patients to unwarranted risk and increases costs to the health care system.
Peter K. Smith, M.D., professor and chief of cardiothoracic surgery at Duke University and co-author of the new criteria, said, “The new ratings that have changed percutaneous coronary intervention (PCI) from inappropriate to uncertain for low burden left main disease, and from uncertain to appropriate for low burden three-vessel disease should result in careful selection of high-risk surgery patients for PCI. Surgeons and cardiologists will now work together to maximize the benefit and minimize the risk for these patients who are at high risk for premature mortality.”
The updated criteria reaffirm that coronary artery bypass is appropriate for patient scenarios with coronary artery disease involving two vessels to include the proximal left anterior decending (LAD) and all variations of three-vessel and left main coronary artery disease. PCI is appropriate in patients with coronary artery disease in all three heart arteries only if the severity of coronary artery disease burden is low. It is uncertain whether PCI is appropriate in patients with three- vessel coronary artery disease and an intermediate to high disease burden. The appropriateness of PCI is also deemed uncertain in patients with blockages in the left main coronary artery, alone or with blockages in other arteries and low coronary artery disease burden. However, PCI is considered inappropriate in patients with blockages in the left main coronary artery with intermediate to high disease burden, according to the new criteria.
“A rating of uncertain does not mean that it’s not reasonable or should not be done,” Patel said. “These are areas where we don’t have definitive evidence and think more research is needed. Remember, the majority of medicine may be considered uncertain by this evidence standard for improvement in health status or longevity. That’s where physicians apply their clinical experience and knowledge to patient care and patients express their wishes.”
For more information: www.scai.org, www.cardiosource.org


 February 06, 2026
February 06, 2026