May 6, 2016 — Atrial fibrillation patients taking warfarin are at higher risk of developing kidney failure if anticoagulation levels are not properly managed, according to a new study from researchers at the Intermountain Medical Center Heart Institute.
Atrial fibrillation is the most common type of heart arrhythmia, which means the heart beats too slowly, too fast or in an irregular pattern. Between 2.7 and 6.1 million people in the United States are living with atrial fibrillation.
Among the most common treatments for atrial fibrillation is blood-thinning medication that prevents blood clots from forming, and thus reduces the risk of stroke or heart attack. Worldwide, warfarin is the most commonly used blood-thinning medication in patients with atrial fibrillation.
Levels of warfarin in the bloodstream are often erratic due to multiple interactions — drug-drug, drug-food and drug-supplement — that result in the need for frequent dose changes to maintain drug safety and efficacy.
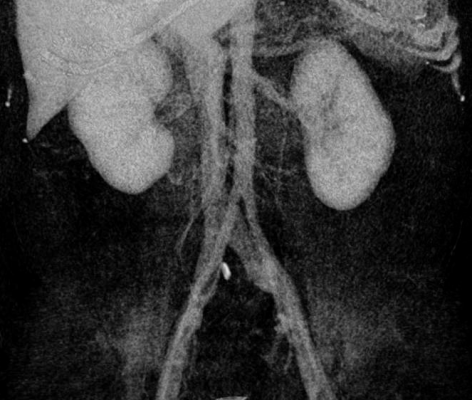
A total of 2,753 patients with atrial fibrillation who were anticoagulated using warfarin and managed by Intermountain Healthcare Clinical Pharmacist Anticoagulation Services — who had a baseline creatinine level of less than 2.0 mg/dL or a glomerular filtration rate greater than 30 and serial renal function studies — were included in the study.
Patients were stratified into categories based on the amount of time their anticoagulation levels were determined to be in a therapeutic range. Researchers then examined kidney health in relation to the amount of time in or out of therapeutic range.
“Our study sought to examine the long-term kidney function of patients who were prescribed warfarin therapy as part of their atrial fibrillation treatment, and who were closely monitored by our Clinical Pharmacy Anticoagulation Service,” said T. Jared Bunch, M.D., director of heart rhythm research at Intermountain Medical Center Heart Institute in Salt Lake City.
Results of the study were presented during the Heart Rhythm Society’s (HRS) 37th Annual Scientific Sessions, May 4-7, 2016, in San Francisco.
If anticoagulation levels are too high, a patient is at risk of hemorrhaging. If the levels are too low, the patient is at risk for developing blood clots that may cause a heart attack or stroke.
These bleeding and clotting events can develop in any organ in the body. In this regard, precise use of anticoagulants in patients with atrial fibrillation is needed to minimize risk of organ injury.
“We learned several important lessons. First, anticoagulation is very important for the long-term kidney health of atrial fibrillation patients,” said Bunch. “Patients who had low times in therapeutic range — which is defined as the safe zone of anticoagulation — experienced significantly higher rates of kidney dysfunction and ultimately kidney failure. Second, all patients were at risk of developing kidney dysfunction, including those who started with healthy kidney function and those who started with moderate-severe kidney disease.”
Heart and kidney dysfunction are often correlated with each other, meaning if the function of either organ begins to decline, the other may be adversely affected, causing further organ damage. Research shows that approximately 18 to 20 percent of patients who have chronic kidney insufficiency have atrial fibrillation.
“Patients who use warfarin as part of their anticoagulation treatment for atrial fibrillation should have their anticoagulation levels closely monitored to ensure proper levels,” said Bunch. “Those who have erratic levels of warfarin despite close monitoring and care should consider other approaches such as newer anticoagulants that have more predictable blood effects, even if they have moderate kidney disease, and non drug-based methods to lower clot risk with atrial fibrillation.”
Other members of the Intermountain Medical Center Heart Institute team included: Heidi May, Ph.D.., MSPH; Tami Bair, RN; Victoria Jacobs; Brian G. Crandall, M.D.; J. Peter Weiss, M.D.; Jeffrey S. Osborn, M.D.; Charles Mallender, M.D.; John D. Day, M.D.; Jeffrey L. Anderson, M.D.,; Jeffrey L. Olson; Katie Johanning; Yenh Long; Scott M. Stevens, M.D.; and Scott C. Woller, M.D.
For more information: www.hrsonline.org

 August 28, 2023
August 28, 2023