Every second counts when someone is having a stroke and immediate care can mean the difference between life and death. While there is widespread consensus on the importance of identification and immediate care for acute stroke patients, a gap remains in the critical role of post-stroke care and secondary stroke prevention strategies. These critical matters impact the care of the more than 795,000 people in the United States who experience a stroke every year. It is estimated that one in four stroke survivors will experience a second stroke within five years[i][ii]. Alarmingly, more than one-third of second strokes are fatal – making post-stroke care and prevention crucial[iii].
Cryptogenic strokes (CS) are strokes of an unknown cause and account for 35% of all strokes.CS is defined as cerebral ischemia of obscure or unknown origin and often occurs when a blockage in a blood vessel reduces blood flow to the brain. Sometimes, atrial fibrillation (AF), a type of arrhythmia or abnormal heartbeat, can cause strokes and demonstrate similar blockages to those encountered in CS. CS patients are typically treated with anti-platelet therapy medications but, as prefaced, if AF is discovered, their treatment plan changes to long-term anticoagulation.

When it comes to detecting AF in stroke patients, short-term monitoring often isn’t enough since AF can be asymptomatic or happen intermittently. Cryptogenic, large-vessel, and small-vessel stroke patients can be ideal candidates for continuous, long-term arrhythmia monitoring, with insertable cardiac monitors (ICMs). Data shows undetected paroxysmal AF can be found in up to 30% of CS patients and 21.7% of large- and small-vessel stroke patients at three years post-stroke[v][vi]. An ICM provides continuous monitoring and heart rhythm data to the stroke care team, to help inform secondary stroke prevention strategies, providing patients with the critical care needed following a stroke.
Previously, ICM procedures were performed only by cardiologists, and many patients were discharged without receiving an ICM due to the unavailability of implanters. Subsequently, these patients were sometimes lost to follow-up. At SUNY Upstate Medical University in Syracuse, New York, the Cardiology and Neurology departments formed a workgroup to identify ways to improve patient outcomes while maintaining a streamlined and agile approach.
A New Path for Stroke Care
Initial implants of ICMs began in 2017 at SUNY Upstate, but the previously established CS program was facing several challenges following staffing changes. At the time, the ICM procedure was dependent on a singular implanter and lacked the infrastructure to allow for multiple implanters in a more collaborative program. This limited the number of patients who could receive access to continuous, long-term monitoring after suffering a stroke.
Qualifying patients had a few options:
- Remain in the hospital for an extended period until the physician is available to implant.
- Go home with a short-term external monitor (like a patch or 30-day Holter), or
- Return to the hospital for the cardiac monitor to be inserted later

SUNY Upstate is located in central New York and receives stroke patient referrals from more than 10 hospitals across the state, making it difficult for patients to return later for additional follow-up and monitoring. Some patients would have to travel several hours from across the state to have the procedure performed in an outpatient setting in Syracuse, which created a significant barrier to access. Once implanted, however, patients could be followed by their care team remotely.

In 2022, vascular and interventional neurologist Dr. Hesham Masoud revised the stroke program’s CS pathway in close collaboration with cardiologist Dr. Andrew Weinberg. They were faced with several challenges including limited inpatient availability, scheduling difficulties with outpatient procedures due to geographic or rehabilitation constraints, and the ever-present insurance denials.
Empowering allied health professionals and advanced practice professionals
To advance the program, the team re-examined the current strategy and shifted focus to improving efficiency and sustainability. Subspecialty collaboration between Neurology and Cardiology was identified as a critical opportunity. Additionally, efforts were made to increase the number of trained ICM implanters to improve patient access to long-term cardiac monitoring. Stephanie Loveless, MSN, FNP-C was the first trained Neurology APP under the supervision of Dr. Weinberg and Dr. Masoud. After completing the appropriate training, Nurse Practitioner, Taylor Weber, FNP-Cin Neurology received credentialing to implant ICMs. This helped minimize the need to rely on the heart and vascular center or procedure room, allowing for implantation at the bedside and same-day discharge using staff on the Neurology floor.
 SUNY Upstate held a collaborative training in the SIMULATION Lab for both Neurology, Cardiology, and Hospitalist APPs to review and simulate the performance of ICM implantation including sterile technique, patient counseling and obtaining informed consent, patient site prep, and sterile field setup. A mannequin paired with tabletop task trainers for simulation of the procedure steps was used and voiced from the control room. This helped address questions asked during the procedure, implantation training, and suturing. The session included a review of relevant order sets and documentation in the electronic health record.
SUNY Upstate held a collaborative training in the SIMULATION Lab for both Neurology, Cardiology, and Hospitalist APPs to review and simulate the performance of ICM implantation including sterile technique, patient counseling and obtaining informed consent, patient site prep, and sterile field setup. A mannequin paired with tabletop task trainers for simulation of the procedure steps was used and voiced from the control room. This helped address questions asked during the procedure, implantation training, and suturing. The session included a review of relevant order sets and documentation in the electronic health record. 
By growing the program’s team and empowering nursing staff to perform procedures at the bedside with additional training, Dr. Masoud and Dr. Weinberg were able to make incremental strides leading to clinical system-wide improvements and efficiency. As a result, the SUNY Upstate stroke program saw an increase in patient access prior to hospital discharge, broader utilization of long-term cardiac monitoring, and improved communication between Neurology and Cardiology services.
How It Works
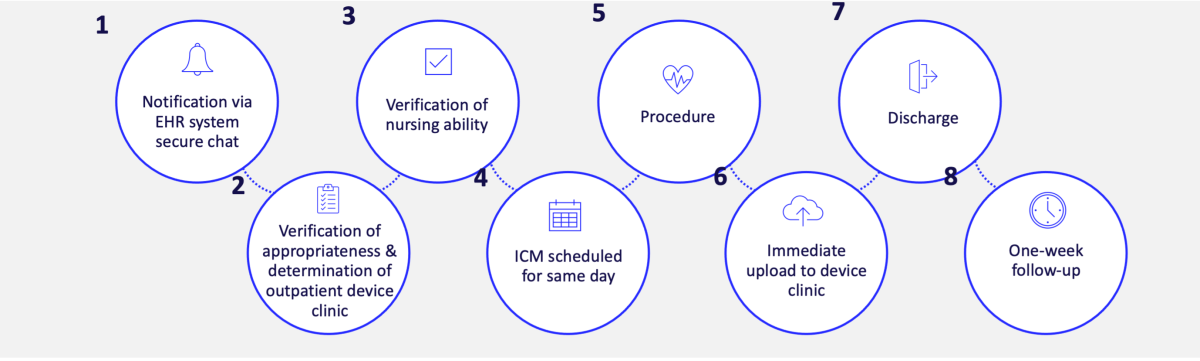
When a patient is diagnosed with a cryptogenic stroke, SUNY Upstate implements the inpatient program care pathway. The first step taken is a notification via the hospital’s electronic health records (EHR) system secure chat, which leads to verification that the patient is an appropriate candidate for an ICM procedure, and determines the outpatient device clinic. From there, nursing availability is verified, and the ICM procedure is scheduled for the same day, prior to discharge. Once the procedure is complete, there is an immediate upload to the device clinic and the patient is discharged usually the same day. Patients are then seen one week after the procedure for a check-up and then followed remotely. This established pathway of care has had a positive impact and is continuing to change the way the system cares for stroke patients.

Enhancing Patient Care
While stroke care pathways have evolved, so too, has medical device technology. Some ICMs are compatible with enhanced, novel AI algorithms, providing smarter, more actionable data. The device is about one-third the size of a AAA battery and is inserted just beneath the skin in a minimally invasive procedure, right near the patient’s heart.
SUNY Upstate is one of the first CS programs in the country to incorporate implanters in Cardiology, Neurology, and Hospital Medicine. Collaboration between subspecialties not only provides opportunity for increased healthcare capacity, but also can reduce healthcare provider burden and offers cost savings. There has also been a positive impact on patient access to care as the number of patients able to receive an ICM prior to discharge has increased substantially. There have been 85 ICMs implanted at SUNY Upstate since March 2024 and several have detected AF.
“The cryptogenic stroke pathway program at SUNY Upstate has enabled our team to deliver better continuity of patient workup without lapses or fragmentation, which may occur when monitoring is interrupted or when patients are awaiting outpatient procedures”, said Dr. Masoud. “Our hope is that these improvements will not only help facilitate improvements to bedside care but also contribute to better patient experience and satisfaction.”
Protocols and processes put in place have contributed to increased AF detection and minimized delays in cardiac monitoring. AF can go undetected by in-office telemetry if AF does not occur while the patient is in the office, but it will be picked up on an ICM. Patients who receive an ICM at SUNY Upstate are monitored remotely by the device clinic. Once AF is detected, patients are informed of the ongoing benefit of the device, including continued monitoring, which provides care teams with critical information that can inform treatment plans.
The Future of Stroke Care
Other institutions can learn from the challenges faced by SUNY Upstate and the solutions developed to establish an effective stroke care pathway. Their stroke program re-design took dependence off the single-provider Cardiology-based paradigm and allowed for the expansion of certified implanters, disrupting the status quo and improving patient care.
SUNY Upstate continues to train healthcare providers to perform implants on patients that are within their domain, thus streamlining patient care that is also synergistic to current provider practice. SUNY Upstate is committed to building healthcare capacity for its community through multidisciplinary-led programs to cross-train providers, striving to break down antiquated models of siloed healthcare to facilitate patient access to the best patient care possible.
[i] Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics—2023 update: a report from the American Heart Association. Circulation. 2023;147:e93–e621.
[ii] Mohan KM, Wolfe CDA, Rudd AG, Heuschmann PU, Kolominsky-Rabas PL, Grieve AP. Risk and cumulative risk of stroke recurrence: a systematic review and meta-analysis. Stroke. 2011;42(5):1489–1494. doi: 10.1161/STROKEAHA.110.602615.
[iii] Callaly, E, et al. Rates, predictors and outcomes of early and late recurrence after stroke: the North Dublin Population Stroke Study. Stroke. 2016; 47:244-246
[iv] 2021 Guideline for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline From the American Heart Association/American Stroke Association. Stroke 2021;May 24:[Epub ahead of print].
[v] Sanna T, Diener HC, Passman RS, et al. Cryptogenic stroke and underlying atrial fibrillation (CRYSTAL AF). N Engl J Med. 2014;370(26):2478–2486. doi: 10.1056/NEJMoa1313600.
[vi]Bernstein RA, Kamal H, Granger CB, et al. Atrial fibrillation in patients with stroke attributed to large- or small-vessel disease: 3-year results from the STROKE AF randomized clinical trial. JAMA Neurol. 2023;80(12):1277–1283. doi: 10.1001/jamaneurol.2023.3931.

 July 29, 2025
July 29, 2025 
