August 19, 2022 — Patients with prior COVID may be twice as likely to have unhealthy endothelial cells that line the inside of the heart and blood vessels, according to newly published research from Houston Methodist. This finding offers a new clue in understanding covid-19’s impact on cardiovascular health.
In a new study published today in JACC: Cardiovascular Imaging, Houston Methodist researchers examined the coronary microvasculature health of 393 patients with prior covid-19 infection who had lingering symptoms. This is the first published study linking reduced blood flow in the body and COVID-19.
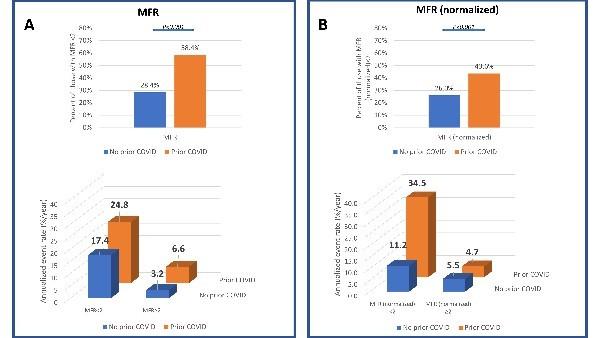
Using a widely available imaging tool, called positron emission tomography (PET), researchers found a 20% decrease in the ability of coronary arteries to dilate, a condition known as microvascular dysfunction. They also found that patients with prior COVID-19 infection were more likely to have reduced myocardial flow reserve – and changes in the resting and stress blood flow – which is a marker for poor prognosis and is associated with a higher risk of adverse cardiovascular events.
“We were surprised with the consistency of reduced blood flow in post covid patients within the study,” said corresponding author Mouaz Al-Mallah, M.D., director of cardiovascular PET at Houston Methodist DeBakey Heart and Vascular Center, and president elect of the American Society of Nuclear Cardiology. “The findings bring new questions, but also help guide us toward further studying blood flow in COVID-19 patients with persistent symptoms.”
Dysfunction and inflammation of endothelial cells is a well-known sign of acute Covid-19 infection, but little is known about the long-term effects on the heart and vascular system. Earlier in the pandemic, research indicated that COVID-19 could commonly cause myocarditis but that now appears to be a rare effect of this viral infection.
A recent study from the Netherlands found that 1 in 8 people had lingering symptoms post-covid. As clinicians continue to see patients with symptoms like shortness of breath, palpations and fatigue after their recovery, the cause of long covid is mostly unknown.
Further studies are needed to document the magnitude of microvascular dysfunction and to identify strategies for appropriate early diagnosis and management. For instance, reduced myocardial flow reserve can be used to determine a patient’s risk when presenting with symptoms of coronary artery disease over and above the established risk factors, which can become quite relevant in dealing with long Covid.
Next steps will require clinical studies to discover what is likely to happen in the future to patients whose microvascular health has been affected by COVID-19, particularly those patients who continue to have lingering symptoms, or long COVID.
This work was supported, in part, by grants from the National Institutes of Health under contract numbers R01 HL133254, R01 HL148338 and R01 HL157790.
Fr more information: https://www.houstonmethodist.org/
Related COVID Content:
COVID-19 Fallout May Lead to More Cancer Deaths
Kawasaki-like Inflammatory Disease Affects Children With COVID-19
FDA Adds Myocarditis Warning to COVID mRNA Vaccine Clinician Fact Sheets
CMS Now Requires COVID-19 Vaccinations for Healthcare Workers by January 4
Cardiac MRI of Myocarditis After COVID-19 Vaccination in Adolescents
Small Number of Patients Have Myocarditis-like Illness After COVID-19 Vaccination
Overview of Myocarditis Cases Caused by the COVID-19 Vaccine
Case Study Describes One of the First U.S. Cases of MIS-C
NIH-funded Project Wants to Identify Children at Risk for MIS-C From COVID-19


 January 28, 2026
January 28, 2026 









