Rupa Sanghani, M.D., FASNC, director of Rush's nuclear cardiology and stress laboratory, explaining to ASNC 2019 attendees how Rush implemented its program during a tour of its PET-CT suite.
As hospital imaging departments look to replace aging nuclear scanners with updated technology, many are asking if cardiac positron emission tomography (PET) might be a better option over the traditional single photon emission computed tomography (SPECT) systems. There are several factors to consider when evaluating PET versus SPECT, including costs, speed, exercise versus pharmacological stress, access to radiotracers and what addition information PET can offer for a more precise diagnosis.
While SPECT remains the workhorse of nuclear myocardial perfusion imaging (MPI), PET offers new imaging options and some centers are looking at installing at least one system to add additional capabilities to their nuclear imaging programs.
At the 2019 American Society of Nuclear Cardiology (ASNC) annual meeting last fall in Chicago, several sessions centered around the uses of cardiac PET and how to create a cardiac PET program.
Advantages of Cardiac PET
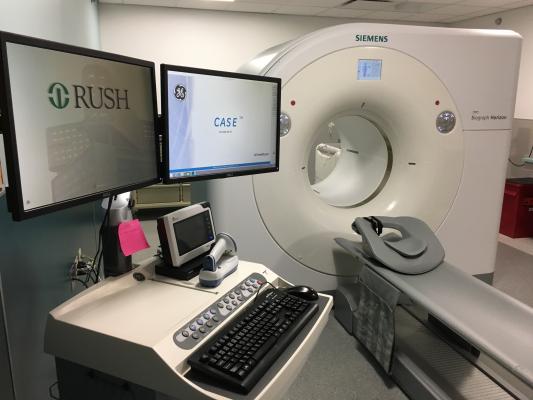
The Rush Medical Center PET-CT system room.
Rush University Medical Center in Chicago recently installed a new PET-CT system and led a tour of its nearby facilities for ASNC conference attendees. Rupa Sanghani, M.D., FASNC, director of Rush's nuclear cardiology and stress laboratory, spoke in several sessions to explain how Rush implemented its program.
There is increasing interest in PET because of its superior image quality and speed over SPECT, and the access to PET radiotracers is increasing. There are new PET tracers in development that are expected to further increase image quality and extend imaging times beyond its current short imaging window. Longer duration tracers will enable the use of exercise stress. Current PET tracers are limited to a 75 second half life, which enables fast exam times, but requires the use of pharamcological stress over exercise stress.
Sanghani said the 75-second imaging time can help increase the number of exams a center is able to perform each day, which was attractive to a high volume center like Rush. She said exercise stress is the preferred method for stress nuclear scans, but some patients, such as those who cannot tolerate exercise or have issues preventing them from using a treadmill, are better suited to pharmacological stress. She said Rush now sends all its pharmacological stress exams to PET.
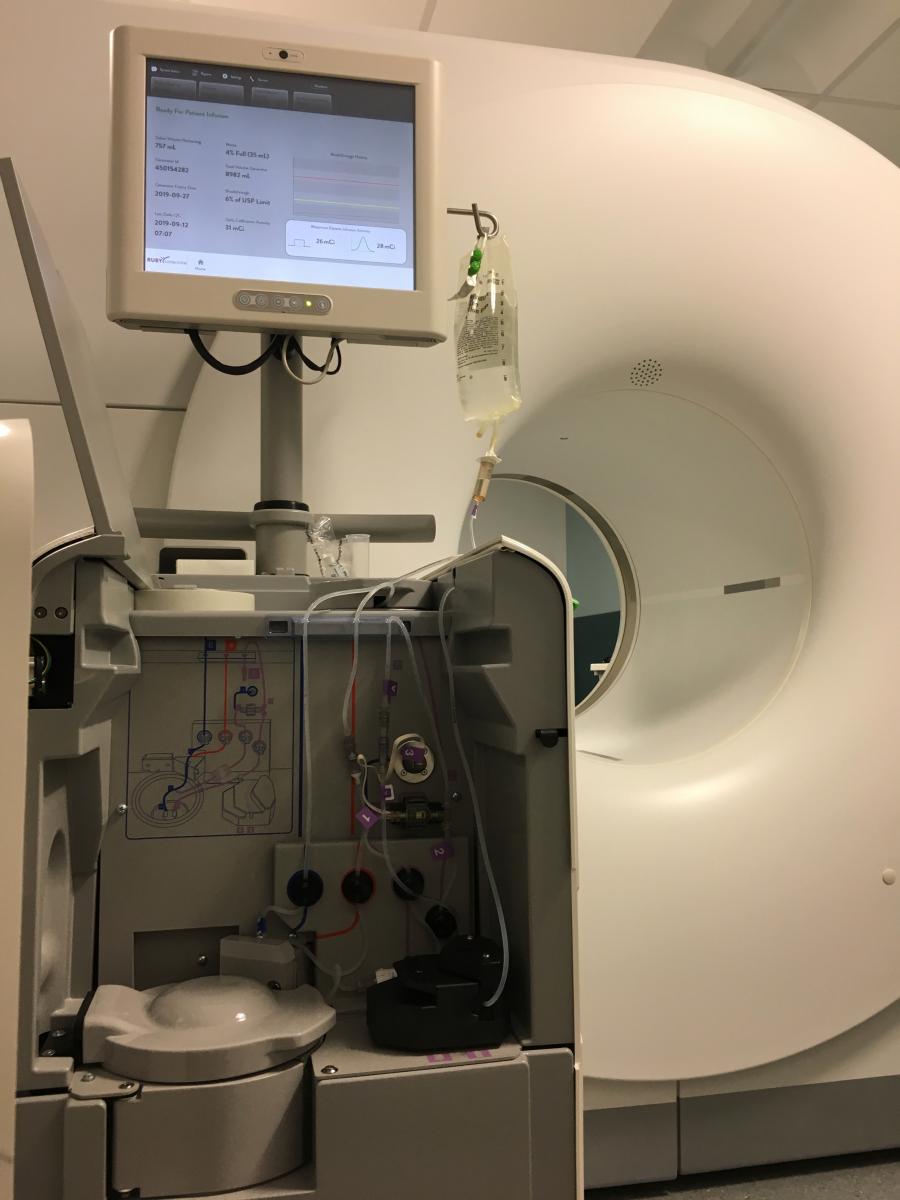
According to Sanghani, another advantage of the short PET half-life of the Rb-82 tracer Rush uses is that it requires it to be auto-injected into the patient during the scan. This eliminates the need for prior injection and a waiting period for myocardial uptake. This means that PET scans can virtually eliminate radiation exposure to staff from the radiation emitted from the patients.
The newer technology for quantitative myocardial perfusion (QMP) flow reserve was also attractive to Rush. Sanghani said it can show the severity of the ischemia detected on a PET scan, determine its cause and help determine the best course of therapy. Additional information from QMP assessments also helps referring physicians better understand the source of ischemia and the next course of action, either medical therapy or interventions.
Computed tomography (CT) is used for PET attention correction, but the CT scanner also can be used to add additional information on the patient. Rush purchased its PET-CT system with a 16-slice CT option. Rush uses it to perform CT calcium scoring exams, adding a risk assessment for future cardiovascular events. The 16-slice system was also picked because Rush did not need a high resolution CT; it already has dedicated high slice scanners for that type of imaging. Cost was also a constraint, but Sanghani said a 16-slice CT was more than adequate for calcium scoring.
 She said PET might be best suited for higher volume centers because of its fast speed. "If you are doing a large volume of pharmacological SPECT stress exams, this is absolutely more efficient," Sanghani said. "PET is a 30 minute scan rather than a three hour SPECT scan, so it is much faster throughput."
She said PET might be best suited for higher volume centers because of its fast speed. "If you are doing a large volume of pharmacological SPECT stress exams, this is absolutely more efficient," Sanghani said. "PET is a 30 minute scan rather than a three hour SPECT scan, so it is much faster throughput."
The Rb-82 radiotracer generator costs around $40,000 and is good for about six weeks before it needs to be replaced. This is an important consideration for centers, because if they have low nuclear patients volumes, PET might not as economical as SPECT, she explained. The photo to the left shows the Rb-82 radiotracer generator located on the back side of the Rush Medical Center PET-CT system.
Improving Myocardial Perfusion Quantification in Nuclear Imaging
One of the newer technologies discussed in sessions at ASNC 2019 was the use of quantitative myocardial perfusion (QMP) 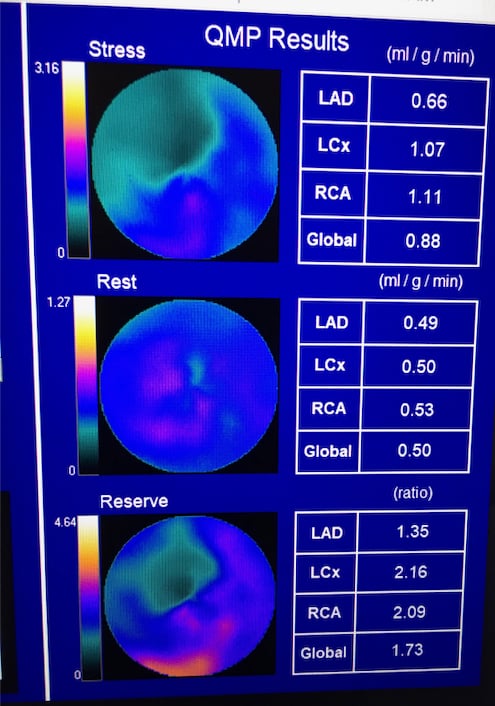 flow reserve to enhance PET imaging. Flow reserve can help show the severity of the ischemia detected on a PET scan and help show its cause and course of therapy. It takes the stress QMP divided by the rest scan QMP to offer a ratio for the flow reserve.
flow reserve to enhance PET imaging. Flow reserve can help show the severity of the ischemia detected on a PET scan and help show its cause and course of therapy. It takes the stress QMP divided by the rest scan QMP to offer a ratio for the flow reserve.
QMP looks at the blood flow in the tissue, not just the heart arteries, at rest and stress. "It looks at blood flow over the continuum, including the epicardia blood flow, which includes everything from the arterials to the capillaries to tissue perfusion," Sanghani said.
The image to the right is an example of PET quantitative myocardial perfusion (QMP) flow reserve imaging.
Planning for a Cardiac PET Imaging Program
Houston Methodist Hospital has a cardiac PET program and Mouaz Al-Mallah, M.D., MSc, director of cardiovascular PET, shared his center's experience at the ASNC 2019 meeting. Beyond myocardial perfusion, the center uses PET to assess myocardial blood flow in post heart transplant patients, for cardiac inflammation imaging and PET/CT fusion to image endocarditis in patients with surgically implanted heart valves.
He said reimbursement is critical to the success of a PET program, so it is very important to have the business side involved early on in building a program to ensure all the reimbursement requirements and documentation needs are met.
Information technology requirements for PET include a gigabit line to transfer data from the machine into data storage/PACS. Al-Mallah said a PET perfusion study is usually between 0.5-1 GB in size.
Rush had a two-year planning process for its PET-CT program. Beyond the new type of camera and radiotracers, they needed to plan for new PET imaging software, new reporting systems, a new ordering system and training staff to read the new modality images.
"One of the most important things is to learn about the modality before you embark on the process of creating a program it is that it is different than SPECT and it is important to understand the subtle nuances," Sanghani explained. "As we went along the process, we asked questions of the vendors and we talked to labs already using PET to see what were some of the pros and cons of the products they used."
She said it is not a seamless transition between PET and SPECT in terms of interpreting images and reporting.
"There is a lot of training required for how to actually process these images for accurate flow quantification and how to interpret these images, the flow and how to incorporate this into reports," Sanghani explained.
She said technologists also need additional training with PET, because it is different than SPECT. Sanghani said it is helpful to identify a couple "super users" for the PET technology and make sure they are really well trained so they can train to other staff after the initial on-site vendor training is over.
For scheduling purposes, Rush uses 45-minute time slots, but the actual set up and scan time take about 30 minutes. "We wanted to make sure we had some cushion in the schedule and even with the 45 minute slots we allotted, we usually can fit in an extra patient without any problems," she said.
Design of a PET Imaging Suite
The PET suite at Rush is designed so staff can be outside the room during the whole procedure to prevent staff radiation exposure. One element to consider is how the patient is put into the bore. Optimally, the control room staff should be able to see the patient's face and the blood pressure monitor, but positioning head first requires the monitor to be on the back side of the PET-CT bore and it is difficult to see the patient.
"We looked at that critically. With the head going in first, the patient's head is actually just outside the bore, which makes them less claustrophobic. If I had put them feet first, their head would be completely in the bore, and I did not think from a motion issue and patient comfort prospective that was going to work as well," Sanghani said.
The issue then became how to see the patient and the blood pressure monitor. They solved this issue by placing a small video camera on the wall behind the scanner so the control room had a clear view.
Shielding a PET-CT room is also a consideration to discuss with a medical physicist. Sanghani said PET requires more shielding than a CT room, and this needs to be included in any build out. "I found our medical physicist on staff to be very helpful to me in the planning," she explained.
If considering the use of F-18 PET agents, the prep area also will need to be lead lined, she said.
Getting Buy-in from Staff on a New PET Scanner
With any type of change, especially using a new technology, you need to get buy-in from the staff that will be working with the new system and the physicians who are referring patients. Sanghani said Rush took a team-based approach that included not only the nuclear imaging department staff and cardiologists, but radiologists, billing experts and the Epic EMR build team. They met weekly for six months leading up to the launch of the system make sure everyone had a say and to address issues as they were brought up.
She said another important consideration is the need to have referring cardiologists document in their order why they need a stress test to aid the pre-authorization of PET exams. She said it is helpful to walk through the documentation process with ordering physicians so they understand what is needed to for PET scan reimbursement. She said it is much easier to get all the information needed up front for insurance processing, rather than trying to gather this information retrospectively.
Building Patient Referrals for a PET Program
"We were a little concerned at first that we would just be shifting patients from SPECT to PET, but we have actually seen our total volumes increase," Sanghani explained. "We are the first cardiac PET program in the state of Illinois. We have started accepting referrals of patients from outside hospitals to provide this imaging modality for patients where you had an equivocal scan, or you want that higher level of information offered by flow qualification."
Al-Mallah outlined patient selection used for PET myocardial perfusion imaging at Houston Methodist, which includes:
• Patients with prior suboptimal or equivocal stress exams;
• BMI of more than 30-35 kg/M2;
• Workup of new heart failure patients who are not optimal candidates for cath; and
• Concern for multi-vessel disease with low ejection fraction.
Related PET Imaging Content:
VIDEO: Practical Considerations for Starting a Cardiac PET-CT Program — Interview with Rupa Sanghani, M.D.
6 Trends in Cardiac Nuclear Imaging at the ASNC 2019 Meeting
VIDEO: PET vs. SPECT in Nuclear Cardiology and Recent Advances in Technology — Interview with Prem Soman, M.D.
Recent Advances in Cardiac Nuclear Imaging Technology
VIDEO: Trends in Nuclear Cardiology Imaging — Interview with David Wolinsky, M.D.
Image Gallery From the American Society of Nuclear Cardiology 2019 Meeting


 January 05, 2023
January 05, 2023