December 17, 2013 — The American College of Cardiology (ACC), along with nine specialty and subspecialty societies, released Appropriate Use Criteria (AUC) for tests used in the
diagnosis and/or evaluation of stable ischemic heart disease. The document assesses 80 potential clinical scenarios with the goal of assisting physician and patient
decision-making. The criteria identify common scenarios in clinical practice and provide a level of appropriateness for the technology’s use based on a risk-benefit analysis.
The criteria are specifically designed to provide actionable standards that can be easily implemented in clinical settings. AUC serves as the foundation for efforts to educate patients through programs like the Choosing Wisely campaign and to engage physicians with ongoing decision support through quality-improvement registries. Establishment of the criteria also facilitates proactive partnerships with purchasers and policymakers to reduce the costs and risks of overuse, audits and prior authorization.
The release of the 2013 Multimodality Appropriate Use Criteria for the Detection and Risk Assessment of Stable Ischemic Heart Disease marks the first time that multiple tests for stable ischemic heart disease have been rated side by side for the same clinical indication. According to the document’s writing committee, the inclusion of multiple testing modalities leverages a greater knowledge base across the tests, promoting optimized decision-making. Consolidation is also meant to eliminate minor differences among the prior single-test criteria.
Partners in development of the document were the ACC, American Heart Association (AHA), American Society of Echocardiography (ASE), American Society of Nuclear Cardiology (ANSC), Heart Failure Society of America (HFSA), Heart Rhythm Society (HRS), Society for Cardiovascular Angiography and Interventions (SCAI), Society of Cardiovascular Computed Tomography (SCCT), Society for Cardiovascular Magnetic Resonance (SCMR) and The Society of Thoracic Surgeons (STS).
“The goal of the document is not to rank order diagnostic tests but to help guide physicians and patients when it comes to making reasonable testing choices amongst the available testing modalities,” said Michael Wolk, professor of clinical medicine, Weill Cornell Medical College, and chair of the writing committee. “These ratings help ensure that tests with the highest potential to benefit are being utilized, while tests are avoided that can cause unnecessary concern and complicated follow-up.”
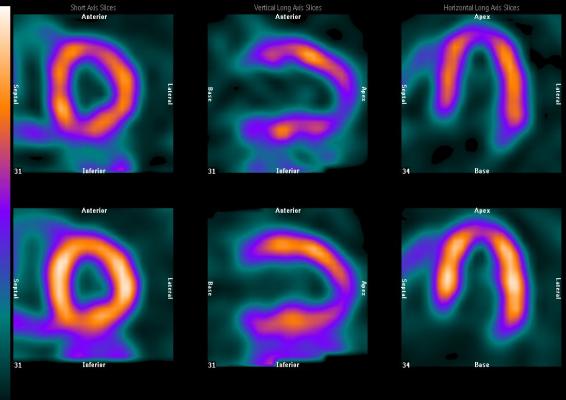
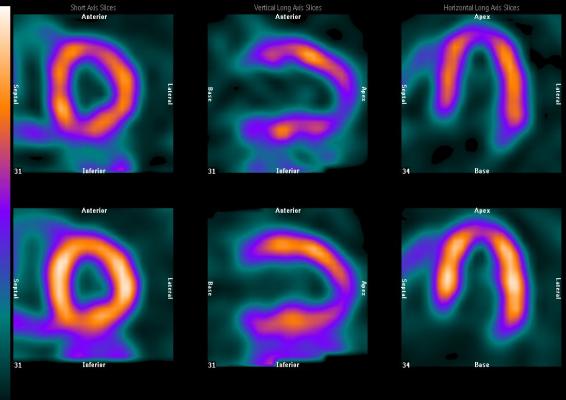
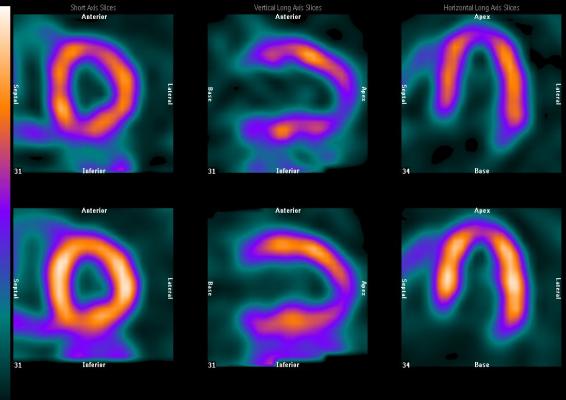
The AUC examine seven testing modalities — both invasive and non-invasive — and rank their use as “Appropriate,” “May Be Appropriate” or “Rarely Appropriate.” The tests include: exercise electrocardiogram (ECG), stress radionuclide imaging (RNI), stress echocardiography, stress cardiac magnetic resonance (CMR), calcium scoring, coronary computed tomography angiography (CCTA) and coronary angiography.
While the current document is the first AUC to incorporate exercise ECG, the other modalities have previously been addressed in their own respective AUC. According to the writing committee, however, new evidence and years of implementing AUC in clinical practice mean that some of the ratings have changed, and the current document should supersede earlier ratings.
Thirty-seven of the scenarios were rated differently from their previous single-test AUC documents. For example, six ratings — all for asymptomatic patients — were lower than in previous documents. In the current document, testing in asymptomatic patients was generally found to be Rarely Appropriate, except for calcium scoring and exercise testing in intermediate- and high-risk patients.
Of the 80 scenarios reviewed, 18 were determined to be Rarely Appropriate across all tests. Included among these was follow-up testing — if the individual does not have new symptoms — after a prior test, percutaneous coronary intervention (PCI) within two years or coronary artery bypass grafting within five years.
Preoperative testing for patients with good functional capacity, prior normal testing within one year or those undergoing low-risk surgery was also included in this Rarely Appropriate group.
Many tests in the initial evaluation of patients with symptoms of stable ischemic heart disease were found to be Appropriate or May Be Appropriate for those with an intermediate or high probability of heart disease. Cardiac catheterization and CCTA were found to be Appropriate for patients to confirm disease and determine treatment options after a previous abnormal
stress-imaging test. A test rated as Appropriate is a reasonable option but is not required for all patients given the specific circumstances unique to each patient.
The writing committee noted that these criteria blend clinical experience with evidence-based information to guide high-quality patterns of care while reducing resource use when patient benefit is unlikely.
“In addition to offering guidance for individual patient cases, the application of these criteria will yield insights into patterns of procedure use over time and increase the opportunity for quality improvement,” said Wolk. “It should further be understood that procedures that have been rated Appropriate or May Be Appropriate should be reimbursed when applied in the suitable clinical scenario.”
The ACC has developed decision-support tools and performance modules for physicians, as well as educational materials for patients to help encourage a dialogue about when and how these tests should be used based on these ratings. These resources, along with the full text of the report, can be found on the ACC’s website. The text will also be available for viewing in a future print issue of the Journal of the American College of Cardiology.
For more information: www.cardiosource.org, onlinejacc.org