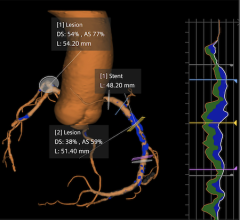
Photo courtesy of Toshiba America Medical Systems Positive remodeling is the most frequent cause of
In the microscopic world of arterial plaque, the only positive thing about positive remodeling is that physicians can visualize it — now noninvasively with multislice detector computed tomography (MDCT) — and treat it before it strikes with deadly force. But early detection of positively remodeled plaque, or the atherosclerotic thickening of vessel walls with outward expansion, is the ongoing challenge cardiologists face, even as 1.2 million Americans suffer a new or recurrent coronary attack each year.
What differentiates the dangerous condition of positive remodeling from negative remodeling (atherosclerotic thickening with inward constriction and stenosis), is its figurative silence. Positive remodeling produces no symptoms, no angina to signal a forthcoming cardiac event, which creates something of a blindfold for physicians in their determination of which patients to evaluate.
“With positive remodeling, there are usually no premonitory signs. This is why people have myocardial infarctions out of the blue without any warning,” said Edward Shapiro, M.D., professor of Medicine at John Hopkins University School of Medicine and director of noninvasive cardiac imaging, Johns Hopkins Bayview Medical Center. “This explains why you can have a negative stress test and then have a heart attack the next day. It’s because with a plaque that is positively remodeled you don’t have any problems with limitations to blood flow. What precipitates the event is a sudden rupture of the plaque. Once it ruptures and causes clots to form, only then does it obstruct blood flow.”
The association of vulnerable plaque with positive remodeling raises the stakes another notch for unsuspecting patients — unstable or vulnerable fibrofatty plaque is covered by a thin fibrous rim; internal hemorrhage in the plaque can result in acute expansion and sudden development of critical lumen stenosis associated with a coronary artery thrombosis, according to Dennis Foley, M.D., chief of Digital Imaging and professor of Radiology at the Medical College of Wisconsin in Milwaukee.
“This explains why 30 percent of patients who suffer from a myocardial infarct (MI) have no preceding symptoms,” said Dr. Foley.
Doctors Shapiro and Foley are among a growing number of physicians who are encouraged by the promise of CT in detecting the occurrence of and link between positive remodeling and vulnerable plaque.
A Viable Alternative?
Literature that supports the use of CT in detecting arterial remodeling is beginning to accrue. In clinical research titled “Assessment of coronary remodeling in stenotic and nonstenotic coronary atherosclerotic lesions by multidetector spiral computed tomography,” led by Stephan Achenbach, M.D., and published in JACC 2004, 43: 842-847, investigators noted that while available data is limited and further study will be required to determine the clinical applicability of MDCT (as well as magnetic resonance), the noninvasive nature of this imaging method makes it “an attractive candidate for further development, especially when the cost and risk of IVUS, the current standard, are considered.”
As the Achenbach article notes, intravascular ultrasound (IVUS) is currently the gold standard method for detecting positive remodeling and visualizing vulnerable plaque. But IVUS is extremely invasive, more so even than catheterization, which is why a noninvasive alterative is so appealing.
“Cardiac CT will have an enormous impact on those patients with undiagnosed coronary artery disease,” said Bruce Lachterman, M.D., medical director for the Cardiac Catheterization Laboratories at Houston Northwest Medical Center and St. Luke’s Community Medical Center, The Woodlands. In a printed Q&A discussion produced by Toshiba Medical Systems (see sidebar, p. 32), Dr. Lachterman said CT enables disease detection beyond coronary artery stenosis.
“Cardiac CT is a breakthrough technology, and I believe it will become the gold standard for cardiac disease detection,” he said.
Adding to that discourse, Steven Gunberg, D.O., clinical assistant professor at University of Colorado Health Sciences Center, reports that CT takes visualization of the vessel wall and plaque characterization to a new plane.
“The 64-slice detector cardiac CT enables us to visualize evolving plaque, or plaque considered vulnerable, far more easily than conventional coronary angiography,” said Dr. Gunberg. “We’re also able to see changes in the coronary vessels during the procedure and follow those changes more accurately than before.”
Vulnerable Connection
Researchers at the University of California, Irvine, School of Medicine, led by Jagat Narula, M.D., highlight the importance of multislice CT (MSCT) in allowing characterization of the composition of plaques, and, perhaps most significant, detection of the large necrotic core, which the team says “is becoming the sine qua non of plaque vulnerability.”
In an article titled, “Picking Plaques That Pop,” the group asserted that progressive enlargement of the necrotic core is associated with [a plaque’s] vulnerability to rupture. It concluded that MSCT should be able to identify large necrotic cores and outward [or positive] remodeling.
“Arterial remodeling of the vessel wall is the most important marker that can set the MSCT apart from angiography since the vessel wall can be easily observed,” the article states.
The connection between positive remodeling and vulnerable plaque is an accepted relationship — where positive coronary remodeling is found, vulnerable, soft plaque is likely to be present, and this is predominantly true in patients who have risk factors for cardiac disease but who have not yet developed clinical manifestations, according to Dr. Shapiro at John Hopkins.
“If you look at the microscopic content of the plaque that is positively remodeled, they contain more inflammatory cells and more lipids,” he said. “Those are known to be markers of plaque instability. The remodeling plaques have features that make them unstable.”
Dr. Shapiro also states that positive remodeling is more prevalent than negative remodeling, and the more common cause of MIs.
Too Soon for Certainty
Despite the promise of CT as a tool to identify positively remodeling vessels, sources are quick to add an important disclaimer to their endorsements. And that, fundamentally, is the absence of clinical evidence — via multicenter randomized trials — to verify the efficacy of cardiac CT in identifying positive remodeling and vulnerable plaque.
“So far, the ability and accuracy of MDCT to determine the extent of coronary remodeling have not been evaluated,” states a portion of the Achenbach discussion.
Many institutions are currently involved in trials to achieve this end, including Johns Hopkins, said Dr. Shapiro. But until results from these studies are available, he says it would be premature to assume that CT can replace IVUS in plaque detection and characterization.
“There are no scientific data yet proving that CT detection is worthwhile, just because it is new,” said Dr. Shapiro. “That is going to require plenty of study. And screening asymptomatic patients will be problematic until CT delivers less of a radiation dose. You shouldn’t subject populations to radiation without proof of efficacy, so screening of asymptomatic people is not yet recommended.”


 February 02, 2026
February 02, 2026