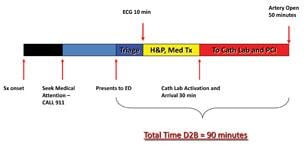
Figure 1: An illustration of the times involved in STEMI treatment, from the onset of symptoms until delivery of reprofusion therapy. The goal of any STEMI protocol is to reduce the time to under 90 minutes.
Heart disease remains the number one killer of both men and women in the United States, with ST elevation myocardial infarction (STEMI) remaining one of the most feared manifestations. The underlying mechanism of a STEMI is plaque rupture and subsequent thrombosis of a coronary artery, causing subsequent myocardial ischemia, which progresses on to myocardial necrosis and infarction. Cardiac myocytes are exquisitely sensitive to hypoxia, and cell death ensues within 60 minutes of artery occlusion. Multiple studies have demonstrated that the sooner the occlusion is relieved and blood flow re-established, the lower the mortality and morbidity of patients suffering from STEMI. For this reason, reperfusion therapy has become the cornerstone of treatment for these patients.
American College of Cardiology/American Heart Association (ACC/AHA) guideline recommendations for the treatment of STEMI provide two choices for reperfusion therapy — medical reperfusion with thrombolytics and mechanical with primary percutaneous coronary intervention (PCI). Because of the short therapeutic window available for reperfusion, current recommended goals consist of a door-to-needle time of 30 minutes or less and a door-to-balloon time (D2B) of 90 minutes or less. The preferred method for reperfusion, where available, is primary PCI, and the rest of this article will focus on this modality.
Keys to a Successful PCI Program
To meet ACC/AHA targets, the clock starts the moment the patient hits the emergency department (ED) door, either by emergency medical services (EMS) or by walking in. Achievement of a D2B time equal to or less than 90 minutes requires a complex interaction between various players — first responders, ED physicians, cardiologists and supporting staff — and also requires a substantial financial and political investment by hospital administration (Fig. 1). Without each part of this complex mix working together as an integrated team, success of any primary PCI program would remain doubtful.
There are several key components of a successful primary PCI program endorsed by both the ACC and the AHA that when adopted have led to significant reduction in reperfusion times:
1. An institutional commitment to accept all STEMI patients regardless of reroute/bypass status
2. 24/7 interventional cardiology and cath lab team coverage
3. Single page activation of the cath lab team — nurses, techs and interventional cardiologist on a single pager
4. ED physician activation of the cath lab, not cardiology activation
5. Multidisciplinary group consisting of ED physicians, cardiologists, nursing, cath lab staff and hospital administration for quality assurance
6. Transfer protocol agreement for primary PCI programs without coronary artery bypass graft (CABG) surgery backup
Aligning These Measures at a Hospital
My personal experience in instituting STEMI programs at the University of Illinois at Chicago, the Jesse Brown VA Medical Center in Chicago and now at the Pali Momi Medical Center in Aiea, Hawaii, has demonstrated the significant impact these simple changes can make in D2B times. They also illustrate the intrinsic barriers and inertia faced with any nascent program.
Before any primary PCI program can be initiated, an institutional commitment by all players involved is essential. Not only is there a significant layout of capital that is required by the hospital — medications, stents, balloons, etc; but also additional hires will be required to ensure adequate coverage of the cath lab. Participating Interventional cardiologists will need to agree on a call schedule and protocol, and strategies for accommodating these patients when the ED or hospital are on reroute/bypass need to be developed.
Single page activation of the cath lab team is a simple and powerful tool to reduce overall D2B times by up to 30 minutes in my own experience. All members of the call team are provided pagers with the same activation number. Pagers with dual activation numbers, one for routine use and one for emergency activation, do exist. Primary responsibility for activating the on-call pagers and confirming callbacks by team members is assigned to a single person using a dedicated STEMI phone line. This person can be the ED clerk/receptionist, the nursing supervisor or the operator. But, it must be the same person every time to reduce confusion, and the same protocol must be used every time for the same reason.
One of the most contentious issues of the new primary PCI protocol recommendations is having the interventional cardiologist on-call relinquish control of cath lab activation. This has been an issue due to fears of incorrect interpretation of electrocardiograms (ECGs) by noncardiologists, leading to an increased rate of false positives. Some fear this can lead to either inappropriate cardiac catheterizations or wasted resources and money having a call team activated without cause. It also has been an issue due to the natural tendency of interventional cardiologists to desire primary control of “their” cath lab. Multiple studies have demonstrated, however, that the diagnostic accuracy of 12-lead interpretation by ED physicians for STEMI is as good as, if not better than, cardiologists. ED activation of the cath lab team has reduced D2B times by up to 60 minutes or more in my institutions.
One vital component of any successful primary PCI program is the establishment of a multidisciplinary team of nurses, cath lab staff, ED physicians, cardiologists and hospital administration, whose sole purpose is to review all STEMI cases and identify areas of improvement and areas that are working well, and will flag any potential errors or system barriers that may be prolonging D2B times.
Primary PCI programs without surgical backup are becoming commonplace across the United States. This is a result of both a decline in cardiothoracic (CT) surgeons and an overall decline in the number of coronary artery bypass surgeries being performed across the country, leading to a reduction in the number of active surgical programs. There is also recognition that primary PCI, when performed correctly, significantly reduces morbidity and mortality, leading to a push to improve access to care for wider areas of the United States.
While current generations of interventional products have made the treatment of most STEMIs a matter of course, the need for CT surgical backup is still very real. A formal agreement with an institution with an active CT surgery program is essential, with a recommended transport time of less than 30 minutes. At the Pali Momi Medical Center, a transfer protocol was developed with The Straub Clinic and Hospital, and actual “dress rehearsals” are conducted at least yearly to ensure adequate coordination between EMS and the participating institutions.
These simple steps, when implemented correctly, can and do lead to significant reductions in reperfusion times. At the programs I have helped start, reductions in D2B times by as much as 50 percent were realized. At The Pali Momi Medical Center, primary PCI was not offered two years ago. In 2009-2010, our D2B rates of less than 90 minutes were only a modest 52 percent. With a firm commitment by all participating players to adhere to the ACC/AHA recommendations, our rates of D2B below 90 minutes reached 92 percent in the 2010-2011 period. Future initiatives to improve our D2B times and improve our delivery of care include field activation of the cardiac catheterization lab by EMS when 12-lead ECGs demonstrate a clear-cut STEMI. We are also formalizing a single-call transfer and cath lab activation by referring hospitals without PCI capability.
Editor’s Note: John Kao, M.D., FACC, is the medical director, cardiovascular services, at Pali Momi Medical Center in Aiea, Hawaii. He is a member of the DAIC Editorial Advisory Board.



 November 14, 2025
November 14, 2025 









