April 8, 2011 — A transcatheter ventricular assist device performed better than intra-aortic balloon pumps (IABP), with a 21 percent reduction in major adverse events at 90 days. This was according to final data from the PROTECT II study, presented this week by William O’Neill, M.D., dean of University of Miami and principal investigator, at the American College of Cardiology's (ACC) Scientific Session in New Orleans.
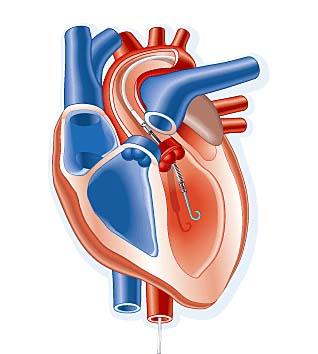
The PROTECT II study was a prospective, multi-center, randomized trial designed to measure a composite of major adverse events at 30 days, with 90-day followup in high-risk percutaneous coronary intervention (PCI) patients requiring hemodynamic support, comparing the Impella 2.5 percutaneous ventricular assist device (P-VAD) to the IABP.
Positive overall outcome for the Impella arm in the entire study cohort at 90 days resulted in a 21 percent reduction in major adverse events over the IABP (p=0.029).
“There was a significant reduction in the major adverse event rate with the use of Impella,” O’Neill said. “I think we learned the device provides superb hemodynamic support.”
He said the PROTECT II study is a major advance that will help guide how interventional cardiologists treat high-risk PCI patients in the future.
“At 90 days, there is a very significant advantage to the Impella-treated patients,” O’Neill said. “As evidenced by this data, this superior level of hemodynamic support in the cath lab allowed for a more complete procedure, leading to a reduction in out-of-hospital major adverse events.”
Most high-risk PCI cases are rushed, emergency situations where restoration of coronary blood flow as quickly as possible is the goal. “This device allows us the luxury to take our time with these procedures,” O’Neill said.
“It was a very positive trial,” said Samin Sharma, M.D., FACC, director of cardiac cath lab and intervention, co-director of the Cardiovascular Institute, Mount Sinai Medical Center, New York, who attended the presentation. “(Impella) allows the interventionalist to do a good job.”
However, for most cases Sharma said IABPs likely will remain the standard-of-care. He believes they provide adequate hemodynamic support in patients with ejection fractions above 20 percent.
“It should not replace the balloon pumps for the majority of cases,” he explained. “But, in patients with an ejection fraction of 20 percent or lower, we should replace the balloon pump with the Impella device.”
The guidelines for device use in the study were ejection fractions lower than 35 percent in patients with unprotected left main disease, and lower than 30 percent in patients with multivessel disease.
First Comparison of VADs vs. IABP
IABPs have been the standard-of-care to increase blood flow since the 1970s. In the past decade, two types of temporary P-VADs were introduced, which appeared to offer more flow than IABPs. However, the cost of a balloon is much less than the cost of a P-VAD.
Abiomed, the maker of Impella and sponsor of the study, hoped the study would show the percutaneous continuous flow pump offered more perfusion and hemodynamic support than IABPs. This is especially important in the niche of high-risk patients with severely compromised cardiac output.
The Impella 2.5 device helps take over 2.5 liters per minute of flow to compensate for patients with dangerously low ejection fractions. IABP manufacturers Maquet and Teleflex say their balloons provide between 0.5 and 1 liter per minute of augmentation support.
The PROTECT II is a landmark study, because it is a first to examine the complexity and advanced disease of the patient population receiving PCI requiring hemodynamic support (approximately 60 percent were turned down for surgery) and the first analysis of use of atherectomy in low ejection fraction (EF) PCI patients. It was also the first FDA premarket approval (PMA) study measuring IABP major adverse events. Balloon pump technology never had to undergo PMA because it was a standard-of-care prior to the FDA creating that review process.
Study Highlights
Overall, O’Neill said myocardial infarction rates were about the same between both Impella and IABP. But stroke and transient ischemic attacks were higher with IABPs.
At the beginning of the trial, Impella had more adverse events than expected, but dropped off later in the study. O’Neill attributed this to a learning curve with using the device at centers unfamiliar with it.
“A balloon pump is a very stable, known strategy, so the adverse event rate was very low,” O’Neill said. “Once the learning curve was pushed, operators became better, there was a significant reduction in the major adverse event rate with the Impella.”
In the pre-specified high-risk PCI without atherectomy subgroup (88 percent of study), Impella provided a significant benefit over the IABP at 30 days (p=0.009) and at 90 days (p=0.003) with a 29 percent reduction of major adverse events. O’Neill said this was mainly due to readmission of patients who received an IABP.
Bleeding and other major vascular complication rates were the same between the two devices.
In the pre-specified atherectomy group (12 percent of study), there was no overall statistical difference (p=0.316) in major adverse events at 90 days. In this subgroup, the Impella arm demonstrated a significant increase in periprocedural CK-MB release (p=0.030) and decreased repeat revascularization at 90 days (p=0.006).
Impella significantly reduced out-of-hospital major adverse events overall by 56 percent (p=0.002) over the IABP arm.
Per the study conducted by an independent economic health organization (n=227), the Impella reduction of major adverse events translated into overall lower hospital charges per patient, ranging from $12,000 (all patients) to $17,000 (survivors only) at 90 days. Abiomed said more economic analysis data will be presented in future healthcare forums highlighting reduced repeat revascularization, lower charges per readmission and reduced critical care length of stay.
The PROTECT II study was prematurely halted in December 2010 per the recommendation of the Data Safety Monitoring Board. This was based on the 50 percent interim enrollment data with the assumption that it would not meet its primary endpoint at 30 days. The treatment effect of Impella over IABP improved during the course of the trial, suggesting a learning curve for the Impella device.
The superior hemodynamic support of Impella appears to have led to significant procedural differences between the two arms. The original study was powered at 80 percent with the intended final population of 654 patients. The interim report included the 50 percent mark, and final analysis included an additional 19 percent of patients. The pre-specified “roll-in subject” analysis demonstrated that, without the first patient in both arms, Impella was significantly better at 90 days (n=307; p=0.027).


 January 05, 2026
January 05, 2026 









