Point-of-care platelet aggregation testing systems, such as VerifyNow from Accumetrics, can quickly determine if a patient will respond to clopidogrel.
Clopidogrel (Plavix) has been the standard antiplatelet therapy for a decade, but it is now facing challenges with the fact that one-third of patients do not respond to the agent and new drugs offer alternatives.
Aspirin, a key antiplatelet agent, is often used in combination with other agents, chiefly clopidogrel. Both help prevent dangerous clots from forming when vulnerable plaques rupture, which can cause a myocardial infarction (MI). Dual antiplatelet therapy is especially important following percutaneous coronary interventions (PCI) to prevent stent thrombosis. The usual length of treatment is three to six months after implantation of bare metal stents and one year for drug-eluting stents.
However, there is also a need to prevent bleeding complications due to the medications. “When we are performing PCI, we have to think about the balance,” said Roxana Mehran, M.D., Mount Sinai Medical Center, N.Y. She directed a Cardiovascular Research Foundation (CRF) course on why bleeding matters at the American College of Cardiology (ACC) 2010 meeting. Mehran said a big question has been whether to take a cardiac patient off clopidogrel prior to elective PCI or surgery to prevent excessive bleeding. To do so increases the risk of MI. She said some studies have shown mortality from major bleeding and MI are about equal.
“We are at war with coronary disease,” said Sunil Rao, M.D., Duke University Medical Center, Durham, N.C., at the same course. “Mortality is the most important endpoint. Bleeding — similar to MI — is associated with increased mortality. Bleeding is a common complication, but reducing bleeding today is achievable with the numerous agents now available.”
Clopidogrel Nonresponders
Researchers have found roughly a third of the U.S. population does not respond to clopidogrel because of a genetic variation in their CYP2C19 enzyme. This can be detected with genetic testing, but this is not practical due to the cost and lack of reimbursement.
“Most people are not going to bother with genetic testing because it is not covered by insurance,” said Kirk Garratt, M.D., MSMB, assistant director of cardiac interventions and clinical director of cardiovascular research at Lenox Hill Heart and Vascular Institute in New York. He said a less-expensive and easier alternative is platelet reactivity testing. This can be performed as a point-of-care blood test in a physician’s office. “Most people see this as a more sensible approach,” he explained.
Nonresponders have a higher risk of stent thrombosis and an increased risk of major acute coronary events, said Matthew J. Price, M.D., of the Scripps Translational Science Institute and Scripps Clinic in La Jolla, Calif. Price said there have not been any large randomized trials to test whether genetic or antiplatelet reactivity testing is best to determine nonresponders. However, he said the advantage of genetic testing is it can be done without the patient being on Plavix, while platelet function testing requires patients to take the drug and be tested several hours later.
The 3,000-patient GRAVITAS (Gauging Responsiveness With A VerifyNow Assay-Impact On Thrombosis And Safety) study showed the ability of using point-of-care antiplatelet reactivity testing. The Accumetics VerifyNow testing system was used to determine Plavix nonresponders and whether doubling the clopidogrel dose overcomes nonresponse. Loading doses were increased and maintenance doses were raised from 75 to 150 mg. The results of the study, released during the American Heart Association (AHA) scientific sessions in November, showed changing the dose has no effect.
“It did not make a lick of difference,” said Garratt, who participated in the GRAVITAS study. Double-dosing was expected to lower the cardiac event rate, but he said it made no difference what amount of drug was administered.
“The GRAVITAS findings do not support a uniform treatment strategy of high-dose clopidogrel in patients with high residual platelet reactivity based upon a single platelet function test after stent implantation,” said Price, who served as the study’s principal investigator. “This is important, as currently many physicians utilize a strategy of doubling the dose of clopidogrel the morning after the stent procedure. Alternative therapies or testing a patient multiple times to treat to a specific target of reactivity deserve consideration.”
Price uses the VerifyNow test to help adjust antiplatelet dosing and to determine nonresponders, who he switches to the newer antiplatelet agent prasugrel (Effient).
“Folks are charmed by the idea they can perform a point-of-care test and have more information, but you have to be willing to make the switch in medication,” Garratt said. He is not sure all physicians are comfortable with completely switching a patient’s medication. There is no effect of genetic variation in CYP2C19 on the pharmacokinetics of prasugrel or its inhibition of platelet aggregation.
Prasugrel’s Market Impact
Many thought prasugrel would replace clopidogrel when it entered the market in late 2009. “When Effient was released, most people thought this was going to be a game- changer,” Garratt explained, but added this has not happened.
The drug has no interactions with proton pump inhibitors (PPIs), which some research shows may affect the metabolism of clopidogrel. Prasugrel is also a more effective anticlotting agent and even works on clopidogrel nonresponders. “It’s better for patients because of all the things we worry about,” Garratt said.
However, he said the U.S. Food and Drug Administration (FDA) hesitated clearing the drug because trial data showed higher bleeding rates than clopidogrel, which resulted in a prasugrel box warning. Garratt said some physicians look at the switch to prasugrel as a trade-off between better platelet inhibition and a potential to increase bleeding.
“I believe it’s a great drug, but many people are afraid of it,” Garratt said.
Lenox Hill converted to prasugrel as its frontline antiplatelet therapy in both the emergency room and in the cath labs. Garratt said this ensures clopidogrel nonresponders receive antiplatelet benefit without the need for platelet aggregation testing.
He said clopidogrel has likely remained the gold standard because it is so well established in the market. Garratt said there are many studies examining the drug and it is a known factor, so many clinicians feel more comfortable prescribing it than a newer agent. This might not change in the coming years, as clopidogrel’s patent ends in 2011 and it will be the least-expensive antiplatelet agent as a generic drug.
New Antiplatelet Agents
“What we really need is a new agent,” said Lars Wallentin, M.D., Ph.D., professor of cardiology, Uppsala University, Uppsala, Sweden, who spoke at the CRF course about why bleeding matters. He said such an agent should work as well as prasugrel, but with less bleeding, and believes AstraZeneca’s new agent ticagrelor (Brilinta) will emerge as the new front-line therapy.
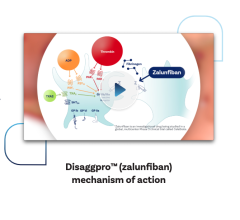
The FDA is currently reviewing a new drug application for ticagrelor, a new compound widely expected to be a big improvement over currently available therapies. The drug is a direct-acting P2Y12 receptor antagonist in a chemical class called cyclopentyltriazolopyrimidines (CPTPs). The agent is the first reversibly binding oral adenosine diphosphate (ADP) receptor antagonist.
Wallentin is a principal investigator in the PLATO (Platelet Inhibition and Patient Outcomes) trial comparing ticagrelor to clopidogrel in 18,624 patients. He said so far the trial data has shown ticagrelor reduced cardiovascular death, MI and stroke and lowered the number of deaths due to stent thrombosis. It offers faster antiplatelet inhibition with lower bleeding risks than prasugrel.
New PLATO findings, presented during AHA 2010, showed ticagrelor may improve outcomes and reduce adverse events better than clopidogrel. Trial data showed ticagrelor significantly reduced the number of days spent in intensive care units after a hospital admission for a heart attack.
However, Wallentin warns there are pros and cons to the agent and more research is needed. “This is a new type of agent with new benefits and new side effects,” he said.
“Ticagrelor is important for several reasons. It’s a pro-drug, so as soon as you swallow it, it starts working — no other process is needed,” Garratt said. P2Y12 inhibitors, such as prasugrel and clopidogrel, first need to be metabolized to be converted into a pro-drug.
Ticagrelor is also reversible. Garratt said the drug’s effect on platelets wears off and the platelets can become active again, which is not possible with clopidogrel or prasugrel. It is also a much more powerful antiplatelet agent, inhibiting about 80 percent of platelet reactivity, as opposed to between 50-60 percent with clopidogrel. While it is more effective, it does not come at the cost of increased bleeding. It has about the same bleeding rate as clopidogrel.
“I think ticagrelor has a leg up on Effient because there is no increase in bleeding rates,” Garratt said.
In clinical trials, ticagrelor also showed a lower mortality rate than clopidogrel, which might be one of its selling points if it is cleared by the FDA. “If a drug representative comes in and says this drug will save lives, people will probably listen,” Garratt said.
The downside of ticagrelor is its short half-life, requiring it to be taken twice a day. Garratt said this could potentially cause patient compliance issues.
Other new agents in development include elinogrel (Portola Pharmaceuticals) and cangrelor (The Medicines Company). Elinogrel is an intravenously injected and oral P2Y12 ADP receptor antagonist. Garratt said the drug works very quickly and is reversible. It has completed phase II trials.
Cangrelor is an intravenously injected, reversible, short-acting P2Y12 platelet receptor antagonist. It is undergoing trials to test its safety in patients undergoing cardiovascular bypass graft surgery.




 January 28, 2026
January 28, 2026