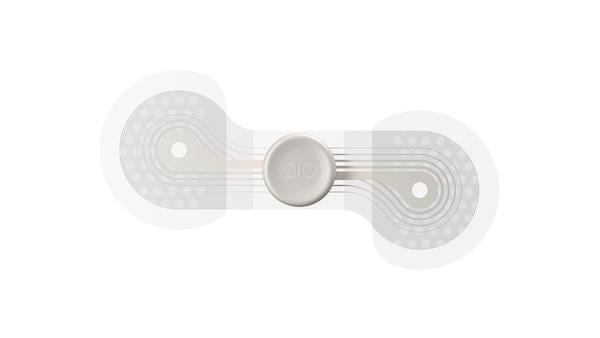
Zio from iRhythm provides long-term (14-day) continuous monitoring.
Patients with type 2 diabetes (T2D) and chronic kidney disease (CKD) are at elevated risk for cardiovascular disease.1 Yet arrhythmias like atrial fibrillation (AFib), which are one of the biggest predictors of heart disease, remain silent until patients suffer a major adverse cardiovascular event (MACE) such as stroke or heart failure.2 Despite this reality, routine screening for arrhythmias is uncommon in most diabetes care pathways.3
Now, researchers are beginning to shed light on how cardiologists can potentially identify and treat asymptomatic and presymptomatic arrhythmias sooner. Two large-scale studies conducted by iRhythm Technologies Inc. and presented at the American Diabetes Association’s 85th Scientific Sessions in June, reveal that arrhythmias frequently emerge before a MACE in patients with T2D and CKD. These data suggest that earlier rhythm monitoring in this high-risk group could uncover problems before they lead to a stroke or heart failure.
Revealing a 'Blind Spot'
In the first analysis, researchers examined a cohort of 8.8 million adults with T2D, including 1.1 million diagnosed with major arrhythmias. Nearly half (47%) of arrhythmias were detected after the initial diabetes diagnosis, with a median interval of 496 days. Among patients who experienced a MACE, 25% did so on or after arrhythmia detection, while 45% took place beforehand.4

The second analysis examined 3.2 million patients with T2D who later developed CKD. Of those, 21% experienced a major arrhythmia, with 59% of those events occurring before the CKD diagnosis. Notably, 17% of patients who suffered a MACE did so within three days of their arrhythmia event.5
“These two abstracts call attention to a blind spot we’ve had in cardiology,” says Mintu Turakhia, MD, a cardiologist and Chief Medical and Scientific Officer at iRhythm, who oversees the company’s scientific research. “Now we can look upstream at the root cause of elevated risks for heart attack, hypertension, and stroke in T2D and CKD patients—arrhythmias and AFib—and find opportunities.”
Beyond Symptom-Driven Detection
Finding arrhythmias through symptoms alone has long been challenging for cardiologists. “Pulse checks may not always be effective because arrhythmias are often paroxysmal and fleeting in nature,” Dr. Turakhia says.
Additionally, people with T2D and CKD may have additional underlying conditions, such as cardiac autonomic dysfunction and cardiac neuropathy, that make them less aware of their heart-related symptoms. “Other times, patients may not be able to articulate their symptoms well,” Dr. Turakhia says. “Some patients may describe having ‘brain fog’ that is actually a sign of impaired blood flow to the kidneys.”
Advances in ambulatory cardiac monitoring technology over the past two decades have given cardiologists more and better diagnostic tools to find silent arrhythmias. One of those devices, Zio from iRhythm, provides long-term (14-day) continuous monitoring. Patients using Zio do not have to remove the device to shower or sleep. A peer-reviewed study published in 2024 showed that Zio is associated with the highest yield of clinical arrhythmia encounter diagnosis and the lowest likelihood of retest when compared with similar devices.6
Advancing Improved Outcomes
According to Dr. Turakhia, arrhythmias represent an inflection point in a patient’s cardiovascular health. “AFib is a harbinger of many other things—the progression to heart failure, the manifestation of coronary artery disease, health care utilization, and costs,” he says. “These care escalations can be avoided by identifying arrhythmias up front.”
To that end, Dr. Turakhia and his team are conducting additional research, aiming to predict the health care spend of a Medicare patient over a one-year period based on the diagnosis of an arrhythmia.
“In my opinion, we need to decouple the opportunity to identify arrhythmia from a single outcome like stroke to focus on the broader set of cardiovascular outcomes,” he says. “When we can get to the point where we can find diseases like arrhythmias that can be treated and then estimate their health care trajectory, it becomes very exciting.”
References
- Swamy S, Noor SM, Mathew RO. Cardiovascular Disease in Diabetes and Chronic Kidney Disease. J Clin Med. 2023;12(22):6984. Published 2023 Nov 8. doi:10.3390/jcm12226984
- Turakhia MP, Guo JD, Keshishian A, et al. Contemporary prevalence estimates of undiagnosed and diagnosed atrial fibrillation in the United States. Clin Cardiol. 2023;46(5):484-493. doi:10.1002/clc.23983
- Bhave PD, Soliman E. Should patients with diabetes be routinely screened for atrial fibrillation? Expert Rev Cardiovasc Ther. 2024;22(1-3):5-6. doi:10.1080/14779072.2024.2328645
- Russo P, Nathan R, Jha V, Singh H, Poh J, Boyle K, Wright B, Hendrickson E. Incidence of Cardiac Arrhythmias in Patients with Diabetes: A Real-World Study. Poster presented at: American Diabetes Association’s 85th Scientific Sessions; June 2025; Chicago, IL. https://s205.q4cdn.com/296879096/files/doc_downloads/2025/120-001754-003_DA_2025-ADA-Poster-Incidence-CA_FINAL-Submitted_Qr_eposter-2.pdf
- Russo P, Nathan R, Jha V, Singh H, Poh J, Boyle K, Wright B, Hendrickson E. Incidence and Timing of Major Arrhythmias in T2D and CKD: A Real-World Analysis. Poster presented at: American Diabetes Association’s 85th Scientific Sessions; June 2025; Chicago, IL. https://s205.q4cdn.com/296879096/files/doc_downloads/2025/120-001754-003_DA_2025-ADA-Poster-Incidence-Timing-MA_FINAL-Submitted-QR_eposter-2.pdf
- Reynolds MR, Passman R, Swindle J, et al. Comparative effectiveness and healthcare utilization for ambulatory cardiac monitoring strategies in Medicare beneficiaries. Am Heart J. 2024;269:25-34. doi:10.1016/j.ahj.2023.12.002


 January 29, 2026
January 29, 2026 









