The XVE Left Ventricular Assist System by Thoratec
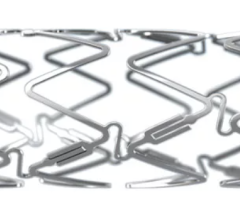
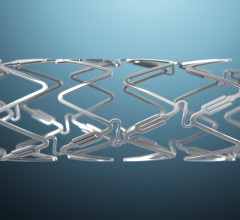
In the simplest of terms, a ventricular assist device (VAD) is a battery-operated mechanical pump that helps a weakened heart pump oxygenated blood throughout the body. While some models offer left, right and biventricular support, others are specially designed to replace the pumping action of only the left ventricle and are appropriately called left ventricle assist devices (LVADs). For those with end-stage heart failure who are awaiting a heart transplant, VADs have been successfully used as a "bridge-to-transplant" therapy. But with continued advances in design and efficiency, the use of VADs as an alternative to transplant is growing. In fact, recent studies have shown that when VADs are used for this kind of "destination therapy," the one-year survival rate of patients with end-stage heart failure is double that of those on drug treatment alone. However, not all VADs currently on the market have been approved by the FDA for use in destination therapy. "There is only one VAD that is approved in the U.S. for bridge-to-transplant that is also used for destination therapy," said Randall Starling, M.D., vice chairman of the Department of Cardiovascular Medicine at the Cleveland Clinic and medical director of the Clinic's Kaufman Center for Heart Failure. As early as 2002 Pleasanton, CA-based Thoratec Corp. had received FDA clearance for its HeartMate line of LVADs that could be used as both bridge-to-transplant and destination therapies. Prior to gaining approval, studies done on 68 end-stage congestive heart failure (CHF) patients who were not eligible for transplants showed that half were still alive a year after being implanted with the HeartMate LVAD, compared to 28 percent of 61 other patients who received only drug therapy. After two years, 27 percent of the HeartMate patients were still alive, compared to only 10 percent of the drug-treated group. Today, the HeartMate XVE Left Ventricular Assist System (LVAS) is the most widely used LVAD, says Margarita Camacho, M.D., surgical director of the Cardiac Transplant and Mechanical Assist Device Program at the Saint Barnabas Heart Center at Newark Beth Israel Medical Center in Newark, NJ. But that model, she notes, will eventually be replaced by the HeartMate II. A next-generation LVAD, the HeartMate II entered Phase I clinical trials in 2004 and Phase II trials in February 2005. Designed for bridge-to-transplant therapy, this LVAD is smaller and, because it uses a rotary pump, has fewer moving parts than the older model. FDA clearance is anticipated for sometime in 2009. Currently in pre-clinical trials, the HeartMate III will be a miniature centrifugal pump LVAD. The device will feature a magnetically levitated impeller with a flow capacity of 12 liters per minute; an integrated "single-fault-tolerant" controller; and a pump that uses the same textured surface as the HealthMate XVE to encourage the formation of a tissue layer as a way to prevent clotting. Design challenges While the newer LVADs offer more options, certain challenges still need to be overcome. "The key is to get a device that's durable, patient-friendly and can be implanted with little risk," said Dr. Camacho. Two major problems have been infections and a high incidence of strokes. The older LVADs, like the HeartMate XVE and the Novacor I use a pulsatile pump with valves that push the blood out in a cycle similar to a regular heart beat, Dr. Camacho says. But the newer LVADs use either axial or centrifugal pumps, which provide a continuous flow of blood out of the left ventricle. In the older LVADs, strokes are caused by blood clots that form in the pump, says Dr. Starling. "Most pumps require anticoagulants because clots can form around the valves," he said. "The advantages of axial and centrifugal pumps is that they have a longer life, are quiet, are more energy efficient and have no valves." Dr. Camacho says that a major problem plaguing the Novacor LVAD is that it had a stroke rate of almost 35 percent caused by clotting inside the pump. "Novacor made three changes in their conduits and brought the stroke rate down to between 10 and 12 percent," she said. "But HeartMate is between three and five percent." Since 2000 the Novacor line of LVADs has been owned by Oakland, CA-based World Heart Corp., which is currently developing Novacor II, a small implantable pulsatile VAD; and the WorldHeart rotary VAD, a small, magnetically levitated, centrifugal, rotary, nonpulsatile VAD. Other companies also are seeing the potential in new designs. In 2005, European approval was granted to the Jarvik 2000 FlowMaker LVAD for use as a bridge-to-transplant therapy and for lifetime use in CHF patients. Weighing only 90 grams, the titanium device uses an axial flow pump. "The industry believes that axial devices will last at least 10 years," said Dr. Camacho. But pumps in which the motor is electromagnetically suspended may last more than 15 years, she adds. And patients using these LVADs may not need any anticoagulants or, at the most, only an aspirin. Early tests show that these devices do not damage blood cells or create clots, she notes. Looking further into the future, Dr. Camacho says LVADs may even be used in conjunction with genetic therapies. "If we combine them with stem cells, there's a potential that new heart cells can develop," she said. "Since a VAD unloads the left ventricle, it produces a restful environment for these stem cells to grow. So this neurohormonal environment is more conducive to muscle regeneration with a VAD in place."





 July 02, 2024
July 02, 2024