May 25, 2023 — First-generation bioresorbable vascular scaffolds (BVS) may be just as effective as drug-eluting metallic stents, which are currently the standard treatment for heart disease patients undergoing percutaneous coronary intervention (PCI).
These are significant findings from a global clinical trial led by a researcher from the Icahn School of Medicine at Mount Sinai. The work could lead to advancements and improvements in new BVS technology and future clinical use among interventional cardiologists across the United States.
This multi-center trial is the largest trial to examine the long-term safety and effectiveness of PCI using Abbott’s “Absorb BVS,” a novel stent made of absorbable polymer (plastic-like material). It shows this treatment option, when properly implanted, may lead to long-term outcomes for heart disease patients that are similar to conventional treatment with metallic drug-eluting stents.
The five-year results from the “ABSORB IV” trial were announced Wednesday, May 17, in a Late Breaking Clinical Trials/Hotline session at the EuroPCR meeting in Paris, the official annual meeting of the European Association of Percutaneous Cardiovascular Interventions (EAPCI), and simultaneously published in the Journal of the American College of Cardiology.
“In this study, the largest ever of BVS in patients with coronary artery disease, the absorbable scaffold, when implanted with optimal technique, resulted in similar five-year rates of patient-oriented adverse events, quality of life, and recurrent angina as the standard metallic drug-eluting stent,” says lead author Gregg W. Stone, MD, Director of Academic Affairs for the Mount Sinai Health System and Professor of Medicine (Cardiology), and Population Health Science and Policy, at Icahn Mount Sinai. “Some adverse events with this thick strut first-generation scaffold were more common within the first three years, prior to its complete bioresorption. Thereafter, event rates were nearly identical with BVS and metallic stents. The early excess risk could likely be eliminated with an improved thinner next-generation scaffold and its implantation with intravascular imaging guidance, affording long-term restoration of the coronary artery to its original native state without a permanent implant.”
Dr. Stone adds, “There is a real desire among patients and their doctors for an absorbable stent which is present early while it is needed and then completely disappears. The favorable long-term results from this study emphasize the fact that this novel technology, which was voluntarily withdrawn from the market by the manufacturer due to lower than expected market adoption, should not be abandoned.”
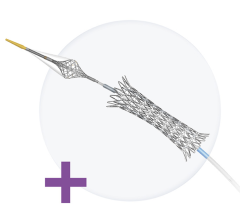
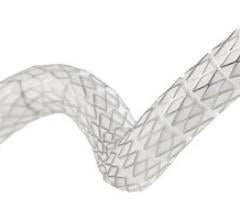
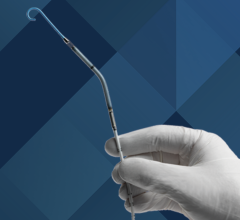
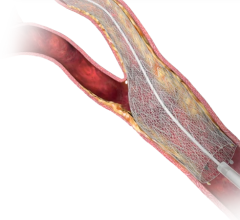
Patients with coronary artery disease—plaque buildup inside the arteries that leads to chest pain, shortness of breath, and heart attack—often undergo PCI, a non-surgical procedure in which interventional cardiologists use a catheter to place stents in the blocked coronary arteries to restore blood flow. The standard treatment uses a metallic drug-eluting stent, and the permanent metallic implant effectively opens the artery. However, the permanent metallic cage may be responsible for the roughly 2 percent per year rate of adverse events that arise from the lesion every year for the life of the patient. Some of these events, known as stent thrombosis events, can cause a fatal heart attack in about 20 percent of cases.
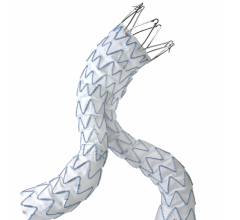
For decades, manufacturers have been working on BVS made of a polymer (a type of plastic) as an alternative. These scaffolds open the blocked artery and then over a three-year period are safely absorbed into the bloodstream, where they are metabolized into carbon dioxide and water. The Food and Drug Administration approved Abbott’s “Absorb BVS” in 2016—the most widely used device of its kind—but the company voluntarily stopped manufacturing and sales.
The ABSORB IV clinical trial compared Abbott’s polymeric everolimus-eluting BVS, implanted with improved technique compared to prior studies, with Abbott’s cobalt chromium everolimus-eluting stents (CoCr-EES) to compare safety and outcomes over the course of five years following the procedure. Researchers randomized 2,604 patients at 147 sites with stable or acute coronary syndromes to receive either BVS with improved technique or CoCr-EES. Patients did not know which stent they received.
At the five-year mark, 17.5 percent of patients with BVS had target lesion failure (cardiac death, heart attack, or repeat intervention linked to the treated device or vessel), compared with 14.5 percent of patients treated with metallic stents—a 3 percent difference. Twenty-one BVS patients had thrombosis (blood clot) linked to the device, compared with 13 metallic stent patients, a 62 percent difference. The risk period for increased cardiac events was within the first three years, before the complete scaffold was absorbed into the bloodstream, but the rates of these cardiac events were similar between both groups from three to five years after implantation. At five years, there was no significant difference between the two groups in death or overall cardiac events, both groups had a similar quality of life (which was measured continually through the five year study period with the Seattle Angina Questionnaire (SAQ)-7 and the EuroQOL-5D Visual Analog Scale (EQ-5D VAS)) and there was no difference in chest pain symptoms.
A unique aspect of the study involved an in-depth look at recurring angina—chest pain—that is often the reason that patients undergo stent implantation. Around 5 to 8 percent of PCI patients typically report this symptom to their cardiologist at any given follow-up time. However, in this trial, researchers had patients in both groups answer detailed questions to characterize their chest pain symptoms continuously for up for five years post-PCI. The descriptions of these symptoms were reviewed by an independent committee to determine whether they were truly angina. This analysis showed 53 percent of patients in both groups (BVS and metallic stent) had recurring angina at some point within five years. This rate, much higher than previously appreciated, may give new insights into the burden of angina on patients and raises questions about the causes of angina.
“The fact than angina recurred so frequently was unexpected, and much higher than we would have anticipated given the fact that the patients and lesions treated in this study were not overly complex. This suggests that there may be causes of angina other than obstructive epicardial coronary artery disease, such as microvascular disease and vasospasm, that require different treatments than stents if we are to further improve patient’s symptoms,” says Dr. Stone.
This study was funded by Abbott.
For more information: www.mountsinai.org

 November 24, 2025
November 24, 2025