March 27, 2012 — The cost to place an implantable cardioverter-defibrillator (ICD) increased by $844 per case after a new requirement from the Centers for Medicare and Medicaid Services (CMS) went into effect in February 2010, which has added little additional benefit for patients. This was according to research presented during the American College of Cardiology's (ACC) 61st Annual Scientific Session this week in Chicago.
That cost, if applied to the approximately 150,000 ICDs implanted in the United States each year, translates to $126 million in additional medical costs. The cost increase results from a new CMS requirement mandating that practitioners providing deep sedation be independent from the practitioner performing an invasive procedure. Previously, nurses administered limited deep sedation under the careful scrutiny of the implanting physician during ICD procedures; now, the implants require an additional physician such as an anesthesiologist.
“There was little evidence to support the policy change with regard to patient safety or outcomes,” said Osama Abdel-Hafez, M.D., an internal medicine resident at the Indiana University School of Medicine and the study’s lead author. “A policy that increases costs significantly without improvement in patient outcomes should be further reviewed.”
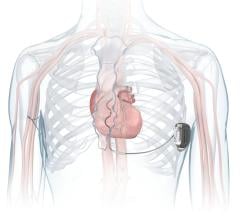
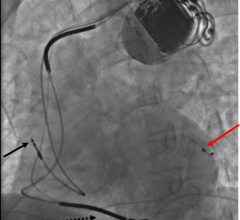
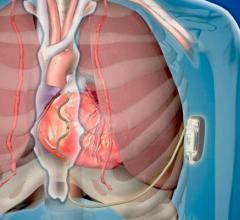
ICDs are small, battery-powered devices implanted in the chests of those at risk for sudden cardiac arrest. If the device detects a dangerous change in heart rhythm, it issues an electrical shock or other therapy to restore a normal heartbeat.
Patients remain conscious throughout most of an ICD implantation procedure, except for a brief period when doctors test the device by shocking the patient, which can be painful and requires deeper sedation.
“Deep sedation is not without complications,” Abdel-Hafez said. “However, there should be better selection of cases that need an anesthesiologist’s services. The CMS requirement was a blanket policy that covered all patients.”
A study from the same research team showed ICD implantation procedures that last longer in duration or that involve specific types of devices, such as biventricular ICDs, have a higher rate of sedation-related complications. Abdel-Hafez said having an anesthesiologist perform the sedation in such cases would make sense. Differentiating between higher- and lower-risk procedures could help improve patient outcomes without imposing unnecessary cost burdens, he added.
The researchers reviewed 431 ICD implants performed at Indiana University Health - Methodist Hospital. Just more than half (243) were performed before the February 2010 policy change; 188 were performed after. After the policy change, patients spent an extra day in the hospital (on average, four days instead of three) and incurred an additional $844 in medical charges per case for a total of $158,000 in additional costs overall.
The study was self-funded by the Indiana University School of Medicine.
For more information: www.acc.org

 January 13, 2026
January 13, 2026