There have been several advancements in
pacemaker technologies over the past few years. This is an overview of some of the most recent advances.
The technologies that will have the most impact on patient care can be grouped into the following areas:
• Tracking device data and patient health through wireless remote monitoring systems;
• Models that are magnetic resonance imaging (MRI)-safe;
• Longer battery life and technology to help reduce pacing requirements to conserve battery power;
• New data recording functionality to provide more information on patient health and device status; and
• The introduction of single-chamber, transcatheter-delivered, leadless pacemaker systems.
About 3 million people worldwide are living with a pacemaker, and each year about 600,000 pacemakers are implanted to treat bradycardia patients.[1]
MRI-Safe Pacemakers
One of the biggest trends in pacemaker technology in the last few years has been the introduction of U.S. Food and Drug Administration (FDA)-cleared MRI-conditional models. These allow patients to undergo MR imaging exams without harm to the device or changes to the device settings. Pacemakers without MRI-conditional use technology usually prevented patients from being able to get an MRI.
More than 6 million people aged 65 or older undergo an MRI scan in the United States every year, and 20 percent of pacemaker patients need an MRI within the first two years of implant, according to Biotronik. According to the Mayo Clinic, approximately 75 percent of patients who have an implantable cardiac device will need an MRI in their lifetime.
Biotronik is the first company in the United States to offer both single- and dual-chamber pacemakers approved for use in an MRI environment. In May 2015, the company reported 60 percent of the pacing devices it sold were MRI-approved, showing the importance of this capability. Biotronik received clearance for its Entovis pacemaker system with ProMRI technology in May 2014, and for its ProMRI Eluna pacemaker system in late March 2015.
“The majority of pacemaker patients are over the age of 65 and most are likely to have a clinical need for an MRI scan after their device is implanted,” said
J. Rod Gimbel, M.D., cardiac electrophysiologist at Cardiology Associates of East Tennessee. “The pacemaker patient population typically has multiple orthopedic, oncologic, neurologic and cardiovascular co-morbidities that are best understood with MRI; thus, it is crucial that we implant pacemakers that allow continued unfettered access to MRI. In my practice, I implant MRI-conditional devices and leads at every opportunity to do so, as I believe MRI-conditional devices are the standard of care.”
In April 2016, Boston Scientific received FDA clearance for a suite of products deemed safe for use in MRI environments. The ImageReady MR-Conditional Pacing System includes the Accolade MRI and Essentio MRI pacemakers, as well as the new Ingevity MRI pacing leads. Patients implanted with the full system are able to receive full-body MR scans in 1.5 Tesla environments when conditions of use are met. The newly-approved family of Ingevity MRI pacing leads includes active and passive fixation models. This marks the first time a passive fixation pacing lead is approved for U.S. patients undergoing MR scans.
The ImageReady System offers automatic daily monitoring via the Latitude NXT Patient Management System. An increasingly important tool for physicians, automatic daily monitoring has been shown to improve survival in patients with pacemakers. The Latitude NXT wireless system allows for earlier intervention and improved patient outcomes by providing physicians with device and patient information through customizable alerts.
In February 2017, Abbott gained FDA clearance for its MR-conditional labeling for both the Assurity MRI pacemaker and the Tendril MRI pacing lead. During an MRI scan, the pacemaker works with Abbott's MRI Activator handheld device to trigger pre-programmed MRI settings appropriately tailored to individual patients. This technology can help eliminate the effort, time and patient inconvenience commonly associated with conventional pre- and post-scan pacemaker reprogramming.
"A long-lasting and small wireless pacemaker that allows patients to undergo MRI scans is an important step forward in growing our available treatment options for patients," said David Sandler, M.D., director of electrophysiology at the Oklahoma Heart Institute in Tulsa, Okla. "The ability to choose a device to best address a patient's cardiac condition no longer has a tradeoff with MRI compatibility. It's the best of both worlds."
Medtronic’s Advisa MRI SureScan pacing systems are FDA-approved for 1.5T and 3.0T full-body MRI scans.
Delaying AFib With Antitachycardia Pacing
Data presented as a late-breaking clinical trial at the 2014 Heart Rhythm Society (HRS) annual meeting showed Medtronic’s Reactive Antitachycardia Pacing (ATP) algorithm in its pacemakers can significantly delay the progression of persistent atrial fibrillation (AF) in patients with bradycardia. Results from the MINERVA (MINimizERight Ventricular pacing to prevent Atrial fibrillation and heart failure) study found that the algorithm reduced the development of persistent AF by a 58 percent relative reduction compared to standard pacemakers.[2]
The algorithm restores the heart back to its normal rhythm by pacing during abnormally fast atrial rhythms. It can slow the progression of the disease by successfully terminating atrial tachycardia/AF episodes. Patients benefiting from the advanced pacing also showed a 52 percent relative reduction in AF-related hospitalizations and emergency room visits. Reduction of these costly care episodes has an estimated potential to save approximately $1,218 per patient in healthcare costs over a 10-year span.
New Pacemaker Functionality
An example of the capabilities available on the newer, high-end pacemakers is Boston Scientific’s Accolade pacemaker. It provides actionable data that may enable earlier interventions. It offers a new atrial arrhythmia report that provides a comprehensive view of the patient’s AT/AF status and information for assessing AF treatment efficacy. These pacemakers also carry forward the HF Perspectiv System, a comprehensive suite of diagnostics that can provide insight into HF disease progression including respiratory rate trend (RRT). This measurement and tracking of respiration, heart rate variability (HRV) footprint, SDANN, autonomic balance monitor and heart rate trend shows long-term maximum, minimum and average heart rates.
The Boston Scientific Accolade and Essentio pacemakers also offer a new post-operative system test (POST) feature, providing a fully automatic system evaluation to check lead impedances, intrinsic amplitudes and capture thresholds prior to discharge. The devices enable a new snapshot capability for real-time review of electrogram (EGM)/electrocardiogram (ECG) data and pacing threshold test results.
Abbott’s Endurity dual-chamber pacemaker has technology to help reduce unnecessary right ventricular (RV) pacing with beat-by-beat ventricular support to optimize patient safety and support intrinsic heart rhythm. The Ventricular Intrinsic Preference (VIP) technology has been shown to reduce RV pacing and heart-failure hospitalization. The device also uses beat-by-beat analysis to keep output as low as possible to maximize pacemaker battery longevity.
The Abbott Assurity MRI pacemaker uses real-time EGM waveform monitoring and can be set with event markers that precede and follow a specific triggering event. These events can be programmed to automatically record up to 14 minutes of stored EGMs when encountering one or more programmable trigger options.
Improving Pacemaker Battery Life
Vendors have worked on improving battery life in pacemakers and other types of implantable devices. As older pacemaker patients are now living longer, and pacemakers are implanted into younger patients, battery lifespan has become an important topic of discussion, since battery/device replacement requires surgery. Battery life is highly dependent on pacing needs. Some vendors have developed algorithms to monitor the heart in real time and reduce pacing as much as possible to extend the battery life.
Boston Scientific projects the longevity of its latest pacemaker batteries to be about 12.1 years.
Abbott said its Endurity pacemaker technology should have a service life of about 14.4 years. The Abbott Assurity MRI pacemaker is expected to have a battery life of about 9.4 years.
Medtronic’s Advisa DR SureScan has a listed battery lifespan of up to 11.8 years.
Wireless, Automated Pacemaker Monitoring
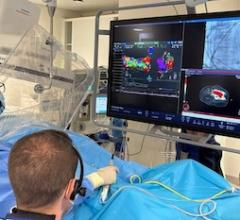
Many of the current generation of pacemakers are equipped with wireless connectivity to external monitoring systems. This can eliminate the need for the patient to come in for office visits just to have their devices interrogated. These systems allow for daily monitoring of device function and the patient’s health status. These remote interrogations allow physicians to monitor patients between infrequent, face-to-face office visits and can alert them to any issues.
In May 2015, the Heart Rhythm Society (HRS) released a consensus statement recommending remote monitoring (RM) systems become the new standard of care for patients with cardiovascular implantable electronic devices (CIEDs).[3] The HRS said over the past decade, several new technologies have created the ability for devices to monitor their own function, record arrhythmias and communicate this information to healthcare providers without participation of the patient. The expert consensus statement included:
• Remote monitoring should be combined with at least an annual in-person evaluation and all patients with CIEDs should be offered remote monitoring as part of the standard follow-up management strategy;
• Before implementing RM, it is recommended that each patient be educated about the nature of RM, responsibilities and expectations, potential benefits, limitations and an explanation of how RM information may be used;
• All CIEDs should be checked through direct patient contact 2-12 weeks after being implanted; and
• Have specific policies in place to govern program operations, roles and responsibilities of those involved and the expected timelines for service provision.
Most of these remote monitoring systems use a bedside base unit that collects and sends the patient information at night when the patient is sleeping. However, vendors are starting to move toward interfacing the implantable devices to mobile devices or the patient’s smartphones to enable constant monitoring.
“The clinical and economic benefits of remote monitoring have been well established over a decade of clinical studies,” stated
Niraj Varma, M.D., in reference to the
2015 HRS expert consensus statement on remote monitoring. “But these benefits are only realized if patients consistently use the technology. When we make the remote monitoring process easy for patients, we increase the likelihood of patient adherence, which has been demonstrated to improve health outcomes.” Varma was lead investigator for the TRUST Trial, which laid the foundation for the guidelines, and co-chair of the HRS committee.
In 2016, Biotronik launched its CardioMessenger Smart in the United States. The portable monitoring device, about the size of a modern smartphone, keeps pacemaker, implantable cardioverter defibrillator (ICD) and insertable cardiac monitor (ICM) patients connected to their physician remotely, enabling more efficient care management anywhere in the world. It automatically transmits vital information from a patient’s cardiac implant to their physician via Biotronik Home Monitoring. This includes daily, automatic reports and fully customizable alerts that can be programmed to the physician’s specifications. The portability of CardioMessenger Smart helps ensure patient compliance and the consistent transmission of data necessary for physicians to identify and prevent potential cardiac events.
The first implantable device to offer a direct interface with the patient’s smartphone for monitoring was the Abbott/St. Jude Medical Confirm implantable cardiac monitor. It was cleared by the FDA in 2017. Experts say this is the first of many new EP devices that will directly link to an app on the patient’s phone. Since patients usually carry their phones all the time, it offers an existing platform that will have much better patient compliance and offer true, 24/7 monitoring of the device and patient’s health.
Leadless Pacemakers
One of the biggest issues with implantable EP devices is the leads that connect the device to the heart. Leads are frequently cited as the weakest component of pacing, implantable cardioverter defibrillator (ICD) or cardiac resynchronization therapy (CRT) due to wearing out or complications due to infection. Traditional implantable devices also require surgery to install the leads and the can, increasing the complexity of the procedure, adding cost and exposing the patient to infection risks. Wireless technologies and the miniaturization of both electronic components and the batteries have enabled the development of transcatheter implantable pacing and now CRT systems, eliminating the need for surgery or the placement of venous leads.
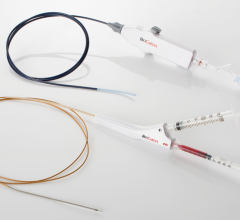
In early 2016, the U.S. Food and Drug Administration (FDA) approved the Medtronic Micra device, the first leadless, catheter-implanted pacemaker approved in the United States. It is the world’s smallest pacemaker at 0.8 cc in size, being a little smaller than its competitor, the Abbott/St. Jude Medical Nanostim. The device has a 20 French diameter and uses a 27 French introducer in the femoral vein, allowing catheter access to the right ventricle. Micra has four self-expanding nitinol hooks that extend as it is unsheathed from its delivery catheter. These act as an anchor, hooking into the trabeculation at the apex of the right ventricle. The operator performs a tug on it to ensure it will not embolize prior to final release. Out of more than 1,600 patients in the post-FDA approval study of the device, there has only been one embolization of a Micra. The battery, while small, is expected to have a 12-year life.
The Abbott/St.Jude Medical Nanostim pacemaker is currently pending final FDA review. The single-chamber pacemaker device is designed to be fully retrievable. It has a docking button on the top of the device which can be grasped by a snare catheter and twisted to turn the device and unscrew the corkscrew-like anchor in the myocardium.
There were recent battery issues with the Nanostim device, causing its distribution in Europe, where it is currently approved, to be paused in 2016. St. Jude said it has now updated the battery technology. The battery life is expected to be nine to 10 years, depending on the pacing requirements for the patient.
It is an 18 French device that is delivered via catheter directly into the apex of the right ventricle. Vascular access is gained through the femoral vein and device guidance is done under angiography.
One issue with these two leadless pacing systems is that they are single-chamber devices, which only account for about 10-15 percent of the U.S. pacemaker market. Medtronic said it views the Micra system as a stepping-stone platform to the next generation of cardiac pacing. This may include the implantation of a Micra pacemaker in each ventricle of the heart and enabling wireless communications between the devices to synchronize their pacing.
“The problem with regular pacemakers is the wire that goes to the heart, because as the heart is beating and the wire has all this motion, over the course of time you can hear breaks in the wires. The idea with a leadless pacemaker is that you take the whole wire out of the equation,” said
Vivek Reddy, M.D., director of cardiac arrhythmia services and professor of medicine, cardiology, Mount Sinai Hospital, N.Y.
Reddy said as a single-chamber pacing system, both the Micra and the Nanostim perform very well according to clinical trial data, and Medicare is now reimbursing use of these devices. He said the main limitation to wider adoption is the single-chamber pacing. “Today, the main limitation with these devices is that we do not have the possibility of doing atrial pacing, and most importantly dual-chamber pacing. These devices are just the first step and the companies are working on ways to do atrial/ventricular pacing,” he explained. “Ultimately, the goal is to avoid the use of a lead, which has always been the weak link in pacemaker systems.”
Related EP Technology Content:
References:
2.
Boriani G, Tukkie R, Manolis AS, Mont L, Pürerfellner H, Santini M, Inama G, Serra P, de Sousa J, Botto GL, Mangoni L, Grammatico A, Padeletti L; MINERVA Investigators. Atrial antitachycardia pacing and managed ventricular pacing in bradycardia patients with paroxysmal or persistent atrial tachyarrhythmias: the MINERVA randomized multicentre international trial. Eur Heart J. 2014 Sep 14;35(35):2352-62. doi: 10.1093/eurheartj/ehu165. Epub 2014 Apr 25.


 January 29, 2026
January 29, 2026