For decades, cath lab clinicians essentially had only one option for achieving hemostasis management following a procedure – compression. That changed in the 1990s with the introduction of vascular closure devices and hemostatic pads, which were designed to significantly shorten the time it took to close the wound left at the access site.
Although compression was – and still is – the gold standard for achieving hemostasis, it often ties up cath lab resources, both in space and staff time. Also, it forces patients to remain immobile for hours at a time. As a result, many doctors are taking advantage of the increasing number of treatment options available to them.
Many Choices
Vascular closure devices (VCDs) such as the Quick-Close system, from Interventional Therapies, often use sutures to close the access site. Although these devices allow patients to become mobile much sooner than is possible with standard manual compression, they are typically much more expensive. Also, some devices leave material behind in the body. However, some newer devices, such as AccessClosure’s Mynx Cadence, use absorbable or dissolvable sealants.
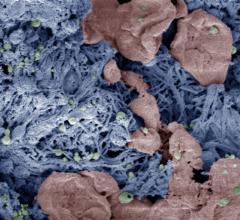
Hemostatic bandages or patches bridge the gap somewhat between manual compression and vascular closure devices. The patches are made with a quick-clotting substance that is used alongside manual compression to significantly reduce the time to ambulation. The patches use a wide variety of substances – derived from marine organisms, seaweed and even clay – to speed up the body’s clotting mechanism.
Magic Dust
Scott Trerotola, M.D., the Stanley Baum Professor of Radiology and chief of interventional radiology at the University of Pennsylvania Medical Center, has been using the BioSeal Advanced powder for more than half a decade. He started using the material when it was sold as an over-the-counter nosebleed control medication and adapted it to help patients in his clinic. It didn’t take long for the powder to win over the clinicians.
“We started using it in a variety of areas and just loved it,” he said. “We got to the point where we started calling it magic dust.”
The powder, which is a mixture of a hydrophilic polymer and potassium ferrate, is placed around
the access site and used in conjunction with manual compression.
Trerotola said his clinic uses the material as an adjunct to manual hemostasis in dialysis access interventions and as an alternative to manual pressure in complicated situations, such as when there is bleeding around a catheter.
Two things in particular about the powder appeal to Trerotola – its safety profile and performance in real-world situations.
“All of our fellows keep a couple of packets in their pockets,” he said. That way, if they come across a patient who’s bleeding from a venous access site, they can quickly close the site in a matter of minutes. Before, Trerotola said a clinician would have to apply manual pressure for up to 45 minutes to stop the bleeding.
Although he doesn’t have concrete data to back it up, he said this has the added benefit of improving the clinic’s room turnover time.
“Instead of standing and holding it there and tying up the room, this clots in a couple of minutes,” he said.
Additionally, in the years he and his staff have used BioSeal Advanced, they have not seen any complications.
“Every now and then it doesn’t do the job, but that’s very uncommon,” he said. “And I’ve never seen a complication related to it. The safety profile is incredible.”
Tried and True
Michael Hallisey, an interventional radiologist with Jefferson Radiology in Connecticut, used nearly every device on the market before settling on QuikClot. He used suture-mediated devices, such as the StarClose system, when they became available in the 1990s, but later switched to the D-Stat and QuikClot hemostatic patches. The closure devices were effective, but Hallisey sometimes experienced complications while using them.
“With the suture-mediated devices, we ran into trouble because sometimes it would tie both sides of the blood vessel and it would occlude,” he said. Results often weren’t much better with plug devices, which Hallisey said would occasionally embolize. But the biggest issue was that often with those devices, clinicians couldn’t re-access a patient for a certain amount of time. However, the patches offered a faster way of getting to hemostasis while being able to rely on the safety and benefits of manual compression. Like with Trerotola, Hallisey’s experiences have shown a very low complication rate along with a low risk of hemotoma.
“We’re seeing a lot fewer complications with hemostasis compression using a QuikClot than we used to have just using straight compression alone,” Hallisey said. “So we think we’ve found the ideal way of doing it.”
After switching, Hallisey said his staff would alternate between using the D-Stat and QuikClot patches. But it turned out that the nurses – the ones actually performing the compression and using the patches – preferred the QuikClot.
“We actually did a little trial in our department with the nurses who were doing a lot of the compression at that time,” he said. “We asked them which one they liked to use because we had them using both, and overwhelmingly the favorite was the QuikClot.”
Not only has QuikClot been preferred by the nurses, it’s been extremely effective. Hallisey said they use the patch for any type of hemostasis management where there’s been some type of puncture. And in his experience, the patch has cut time to ambulation in half.
A Bright Future
Both Hallisey and Trerotola agree that even though improvements could be made, the devices and patches offer advantages to both patient and clinician. Hemostasis times are shorter, complications are often few and far between, and Trerotola points to promising research that suggests BioSeal could even lower the infection rate. Most importantly, though, all the devices help patients get back on their feet faster after a procedure.
“You can’t just get up and walk right away,” Hallisey said. “But you do shorten the time compared to just regular hemostasis.”




 October 27, 2021
October 27, 2021