
Lantheus Medical Imagings Definity perflutren lipid microsphere ultrasound contrast agent
Proponents and researchers of microbubble contrast-enhanced cardiac ultrasound say the technology will eventually evolve to match the diagnostic quality of CT and nuclear perfusion images without the radiation and at a faction of the cost. However, there was an instant chilling effect on the use of contrast-enhanced ultrasound last October when the FDA created a black-box label for all ultrasound contrast agents because of a possible link to increased cardio-pulmonary side effects.
The warning called for physicians using ultrasound contrast agents to monitor patients for 30 minutes following an imaging procedure to ensure there was no adverse reaction. The warning also issued a list of new contraindications. The FDA based its decision on animal studies showing cardio-pulmonary issues related to the use of Sonovue and about 200 serious events recorded in humans. The FDA also said a required post-marketing study of one agent was not conducted by a manufacturer.
Despite the panic these warning created, experts say the agents are safe. They called the FDA decision a knee-jerk reaction to incomplete information.
“This has effected our profession and was thrown onto our practice pretty abruptly,” said Steve Feinstein, M.D., FACC, professor of medicine, director of echocardiography for Rush University Medical Center, Chicago, and a pioneer in the field of echo contrast agents. “It is stifling research and development... There is evidence now that this was bad policy and was an unwarranted move.”
In August, the pharmaceutical and diagnostic imaging marking intelligence firm Arlington Medical Resources reported the black-box warning caused a big decline in the use of injectable ultrasound contrast agents. The report stated echo contrast use declined in the second quarter of 2008 to 22 percent of the usage just two years earlier.
Since the black-label was issued last fall, cardiologists and radiologists have lobbied the FDA to lift the restrictions based on research studies and more than 200,000 retrospective patient case reviews showing there is not a statistically significant difference between patients who underwent contrast and noncontrast ultrasound. They say the benefits of the technology far outweigh any possible risks.
Michael Main, M.D., a cardiologist with Mid America Heart Institute, Kansas City, MO, was among the experts who, along with contrast makers Bracco, GE Healthcare and Lantheus, presented safety data evidence the FDA.
“Multiple studies in 2008 have demonstrated a lack of safety signal in 211,223 patients,” he said, citing two studies he conducted and studies from the Cleveland Clinic and ACC. “There is a lack of any serious adverse events.”
Due to the lobby efforts the FDA pulled back from its initial black-box labeling in July. It removed a number of contraindications from the product labeling and downgraded its alert to a box warning. The FDA now only requires 30-minute monitoring if a patient has pulmonary hypertension. But, the FDA also said in June there is still a need for more research into infrequent serious events, especially with critically ill patients in the ICU.
The black-box warning was a wake up call to many contrast ultrasound proponents who felt an organized effort needs to be undertaken to support the technology and its further development. In September, the International Contrast Ultrasound Society (ICUS) announced its formation during the 23rd annual Advances in Contrast Ultrasound conference (aka the “Bubble Course”) in Chicago. The founders said the group will help spearhead organized education efforts with the FDA to help ensure the technology remains viable in the U.S. The group will also work to foster more research in contrast-enhanced ultrasound. The society welcomes cardiologists, radiologists and those involved with ultrasound imaging for gastrointestinal and medicine and hepatology.
“Combining us altogether gives us a very powerful voice with the FDA and other organizations,” said Lennard Greenbaum, M.D., ICUS Board member and co-director of the Hughes Center for Fetal Diagnostics at Winnie Palmer Hospital for Women and Babies, Orlando, FL.
Using contrast ultrasound
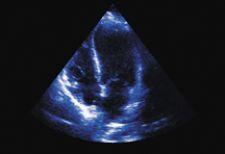
Echo contrast agents include Luminity and Definity by Lantheus, Sonovue by Bracco, and Optison by GE Healthcare. The agents consist of microbubbles made of a lipid shell (a protein shell with Optison) and a non-reactive gas core. The ultrasound waves are reflected off the bubbles, which causes blood or blood-infused tissue to appear much brighter than with ultrasound alone. The ultrasound waves break the bubbles and the shell fragments are absorbed by the liver. The core filler gas is exhaled within minutes. The mircobubble agents are useful for about five minutes of imaging before they start to break down.
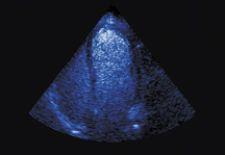
Techniques have been developed to help enhance the diagnostic value of the contrast echo images. Maximum intensity projection imaging uses a time-lapse picture to show vascular density as the bubbles pass through the vasculature and increase the contrast between areas of contrast enhanced blood and tissue.
Pixel intensity threshold analysis (PITA) is a method where an initial image is made prior to administering the agent, then a second image is made seconds later as the contrast agent enters the blood. The background can then be subtracted to create a clearer image of an area of interest.
Ultrasound software can also filter “noise” generated by ultrasound signals to produce clearer images by tracking speckle motion. Speckle tracking is also used to help measure wall motion to detect ischemic tissue.
What the future holds
Roberto Lang, M.D., professor of medicine, director of the noninvasive cardiac imaging lab at the University of Chicago, and a pioneer in the development of 3D echocardiography, said new techniques are being developed for contrast enhanced shape analysis of left ventricle function and perfusion. He said this would allow physicians to better visualize shape changes that occur during a heart attack.
Dr. Lang also said new fusion imaging combining 3D echo with CT or MRI to better visualize obstructions in the coronary arteries is being researched by Philips, GE Healthcare, TeraRecon and TomTec Imaging Systems.
One of the biggest advances for contrast echo in the near future will be its use for myocardial perfusion imaging, Dr. Lang said. “It is at least equal with nuclear perfusion imaging, but the problem is it needs to be proven in large multi-center studies,” he said.
He said these studies are underway and if approved by the FDA, patients could undergo perfusion studies without exposure to radiation. This summer Acusphere Inc. submitted an FDA new drug application for its Imagify polymer microsphere contrast agent designed for perfusion imaging. The NDA includes data from studies of Imagify in more than 1,000 patients worldwide, including two pivotal international multi-center Phase III clinical trials, RAMP-1 and RAMP-2 (Real-Time Assessment of Myocardial Perfusion).
GE Healthcare is developing a new echo imaging agent called Sonazoid that reportedly allows imaging for up to four hours. The agent can also reportedly overcome the stability problems of first-generation microbubbles so it can be used to produce myocardial perfusion images.
GE Healthcare is also working on a speckle tracking system using echo contrast imaging to create a 3D deformable model of the heart. It can be used to measure wall motion and is color coded to show areas of ischemic tissue. Kai Thomenius, Ph.D., chief technologist in the imaging technologies organization at GE Global Research in Niskayuna, NY, said if perfected, the system could compete head to head with nuclear perfusion imaging. He said it would more clearly define the areas of ischemia and be a cheaper and safer system.
“The main thing in the future is these little bubbles will be used as a delivery system for drugs or for diagnosis of specific diseases,” Dr. Lang said.
Research is being conducted to design microbubbles that can attach to specific target cells. This molecular imaging using contrast-enhanced ultrasound relies on the detection of microbubbles retained in the regions of disease. The mircobubble can be modified with targeting ligands (using antibodies, peptides and mimetics, carbohydrates) attached to the bubble shell. Selective targeting of the microbubbles to the vascular markers of diseases has been successful in several animal studies. These studies have used targeted microbubbles to detected inflammation or ischemia-reperfusion injury.
Experiments in clot busting
On the experimental front, the microbubbles that make up ultrasound contrast agents may have a therapeutic use in helping break up blood clots with or without clot-busting drugs.
“The bubbles are smaller than the red blood cells so they can infiltrate the thrombus and can be activated by the ultrasound,” said Evan Ungar, M.D., a University of Arizona professor of radiology and director of cross-sectional imaging.
He said this method works by itself, but can greatly enhance the ability of tissue plasminogen activator (TPA) to clear stroke blockages. However, TPA must be administered in a ridged time window, which accounts for low number of stroke victims when they present to an emergency department and are finally diagnosed. Dr. Ungar said the sonothrombolysis method could be an option for patients who miss the TPA window.
Similarly, Thomas Porter, M.D., internal medicine, section of cardiology, University of Nebraska Medical Center, Omaha, has experimented with noninvasive recanalization of intracoronary thrombi using intravenous microbubbles in pigs. When ultrasound imaging is used to visualize the thrombi and indicate when a large number of microbubbles have entered it, a high-intensity therapeutic ultrasound burst can be used from another transducer to burst the bubbles and help dissolve the clot. He said the ultrasound images can then show the progress of the treatment as the bubbles trickle through the blockage. Dr. Porter said his studies in pigs show recanalization rates greatly improve when ultrasound-guided mircobubble therapy is used.
“Ultrasound and microbubbles can recanalize a thrombosed vessel,” he explained.
Related Echo Contrast Content:
Micro-Bubble Echo Contrast Procedures Rebounded in 2008
Recent Developments and Issues in Contrast Media
Busting Blood Clots in the Ambulance
Ultrasound-Activated Bubbles Aid Clot-Busters
Study Demonstrates Strain Imaging Utility With Contrast-Echo Studies
Study Says Usage of Ultrasound Contrast Agents in Echocardiography Declined
Ultrasound-activated Microbubbles Restore Blood Flow During Heart Attack


 January 28, 2026
January 28, 2026 









