
May 8, 2012 – The team at Texas Children's Fetal Center has successfully completed two in-utero fetal cardiac interventions to treat hypoplastic left heart syndrome (HLHS), a congenital heart defect that is one of the most complex heart defects to treat. The first center in the Southwest to create a program to treat this defect in-utero, Texas Children's Fetal Center and Heart Centers are proud to be able to offer this procedure to future HLHS patients looking for hope for their unborn babies. To learn more about the in-utero fetal cardiac intervention visit http://youtu.be/_VLrfdMq7hg.
"Previously, patients had limited options for their babies when they received an early diagnosis of HLHS during a routine ultrasound," said Michael Belfort, obstetrician and gynecologist-in-chief at Texas Children's Hospital and chairman of the department of obstetrics and gynecology at Baylor College of Medicine. "From this moment on, through the collaborative work of the Fetal and Heart Centers at Texas Children's Pavilion for Women, we can offer more options to families who otherwise would have little hope."
HLHS is a condition that occurs in approximately one in 6,000 live births when the fetus's left side of the heart does not develop normally. Because most of the structures on the left side of the heart are too small and underdeveloped (hypoplastic), it is difficult for the heart to provide enough red blood flow for the body's needs. All children with HLHS will undergo at least three surgeries within the first three years of life. However, if diagnosed early using a fetal ultrasound, some fetuses may be a candidate for the new in-utero catheterization procedure that will help treat HLHS and allow them to be more stable at birth before having to undergo their first heart surgery.
"Thanks to our collaboration with the Fetal Center, our heart program is now so comprehensive that we are in the position to offer care not only to fetuses in-utero but are able to take care of these patients all the way into adulthood. Our expertise ranges across all ages of patients with congenital heart disease," said Daniel J. Penny, chief of cardiology at Texas Children's Hospital and leader of pediatric cardiology at Baylor College of Medicine.
Texas Children's Fetal Center experts have cared for four fetal intervention patients in the last four months. Each case has varied slightly. The first two Texas Children's patients were taken to Children's Hospital Boston where they were treated in collaboration with the Texas Children's team for critical aortic stenosis or a severely obstructed aortic valve. These types of critical aortic stenosis are typically detected mid-gestation and develop into HLHS at the end of the pregnancy. The left side of the heart stops growing and becomes severely underdeveloped, rendering it inadequate to support the systemic cardiac output.
The third and fourth patients were treated at Texas Children's Hospital. For the most recent two patients, physicians were dealing with a rare type of HLHS where the fetus had an intact atrial septum (IAS), a severe congenital cardiac malformation with little possibility of post-natal survival, even with a cardiac intervention performed immediately after birth.
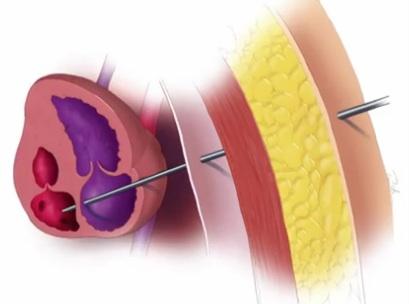
Each complex fetal intervention involved accessing the fetal heart in-utero via a specialized needle and inflating a balloon catheter into the baby's heart. In the first two cases, the balloon was inflated across the fetus' small aortic valve in order to allow blood to be pumped from the heart to the fetus' body. In the last two procedures, the balloon was inflated across the wall between the top two atrial chambers of the heart. The balloon created a hole to allow the passage of blood from the underdeveloped left atrium into the right atrium – a technique that will increase the chances that the baby will have enough oxygen in its blood to survive after birth. In the fourth procedure, a stent was also placed across the wall separating the upper chambers in order to help maintain the opening that was created.
The Texas Children's Fetal Center at the Texas Children's Pavilion for Women is one of only a few centers in the world capable of performing this complex fetal intervention as it involves a coordinated effort among a large, multi-disciplinary team of fetal cardiologists, OB-GYNs, interventional cardiologists, congenital heart surgeons, fetal imaging experts, maternal and fetal anesthesiologists and other clinical specialists. Babies receiving this unique fetal procedure at Texas Children's Fetal Center will continue treatment immediately after birth at Texas Children's Heart Center.
Following each procedure, maternal fetal physicians monitor the mother and baby through multiple fetal ultrasounds and echocardiograms so that the mother may carry the baby to as close to full term as possible, giving the lungs, brain and other vital organs a chance to mature prior to birth.
With this aggressive plan, the hope is that these fetuses will be able to proceed with lifesaving newborn cardiac surgery and subsequently receive a series of three surgeries. The hope for the fetuses who undergo dilation of the aortic valve is that instead of living with only one functional ventricle, the left ventricle is "rescued" in-utero. The goal for these children is that they are born with both the right and the left side of the heart functioning well. For fetuses who undergo opening of the hole between the atrial chambers, the left side of the heart is usually too small to be rescued. These are usually at the highest risk for death shortly after birth. The fetal procedure allows them to be more stable at birth, and to go on to a series of heart surgeries to stabilize the circulation.
The first surgery is a Norwood procedure to reconstruct the heart to allow the right ventricle to become the systemic ventricle and to pump blood to the baby's body and lung. Charles Fraser, chief of congenital heart surgery and surgeon-in-chief at Texas Children’s Hospital, along with his team of cardiovascular surgeons, have a near 90 percent success rate using the Norwood procedure.
For more information: http://women.texaschildrens.org or www.texaschildrens.org/heart



 November 14, 2025
November 14, 2025 









