Photos by Getty Images
By the end of the first year of the COVID-19 pandemic, there was a clear sign that some virus patients had longer-lasting health issues due to their coronavirus infections. There were early studies that postulated there might be long-term myocardial and vascular damage due to COVID, but a year and hundreds of clinical studies later, the impact of long-COVID, or post-acute sequelae of COVID-19 (PASC), appears to be less severe than originally thought.
While there has not been a massive number of new heart failure cases as anticipated in 2020, it is clear that COVID does cause less severe longer-term issues in patients. On the cardiology side this includes chest pain and arrhythmias where the cause cannot be pinpointed. To get a sense of where we are with answers and understanding long-COVID, DAIC spoke with three cardiology experts involved with long-COVID clinics at Cedars Sinai, Mass General and Beaumont hospitals
“While there are still a lot of unanswered questions about long-COVID, I think it is safe to say we have made progress,” explained Aaron Baggish, M.D., director of the cardiovascular performance program, Mass General Hospital. He has been involved in the care of cardiac COVID-19 long-hauler patients and monitoring athletes recovering from COVID the past two years.
Long-COVID also is no longer seen as a big mystery because large numbers of these patients have been seen and treated. The bottom line is that while long-hauler symptoms are an issue for patients, they do not appear to be life-threatening and the big fear of large numbers of new heart failure patients post infection has not materialized.
"Interestingly, the patients do get better. It is a slow process, but by the one-year point we do see improvement in patients with this prolonged syndrome," reassured Justin Trivax, M.D., an interventional cardiologist who works with long-COVID patients at Beaumont Hospital.
Large Number of Health Systems Create Long-COVID Clinics to Monitor and Treat Patients
Healthcare systems realized they needed to collect data to better understand the long-term effects of COVID. Since the fall of 2020, many health systems opened long-COVID clinics to pool resources and objectively evaluate any patients who present with an array of health complaints months after their initial infections that might be due to COVID.
"It has been really incredible to see all these post-COVID clinics open up everywhere," explained Trivax, who became interested in helping with long-COVID patients after he contracted COVID and never regained his sense of smell. "This is really what you need, because not only is this a pulmonary and cardiac disease, but this is probably one of the most multidisciplinary of all diseases I have ever seen."
"I think most tertiary and even community based hospitals are realizing this is an important part of the service line. So I think increasingly patients have resources to use in the face of long-COVID," Baggish added.
These clinics usually include a cross-section of sub-specialists from different departments, including pulmonologists, cardiologists, neurologists, occupational and physical therapists, and other specialists as needed.
"Theses clinics are really helpful because there are too many physicians who are being pulled in too many different directions and don't have the time to sit down with a patient who is really struggling," Trivax said.
Long-COVID Symptoms and Prevalence
"Depending on what study you read, a percentage of patients with acute COVID infection will go on to develop long-lasting sequelae, but typically the percentage falls over time," explained Siddharth Singh, M.D., director of the COVID heart program, staff cardiologist and echocardiographer, Cedars-Sinai Hospital.
He said studies show between 10-25 percent of COVID patients will experience at least one disabling long-COVID symptom six months after their acute infection.
Cedars-Sinai long-COVID has seen over 500 patients since late 2020. Of these, 120 were referred for cardiac evaluations. The most common presentations in those patients include:
• Shortness of breath
• Exertional intolerance
• Chest pain
• Heart palpitations
• Sensations of light-headedness and dizziness
• Insomnia
• Brain fog
• Constipation
• Diarrhea
• Numbness or tingling in the extremities
• Longer lasting issues with smell and taste
Singh also said many patients experience anxiety and depression due to the continued symptoms, and are concerned the issues they have from COVID may be permanent. Both Baggish and Trivax also reported seeing these issues in many of their patients.
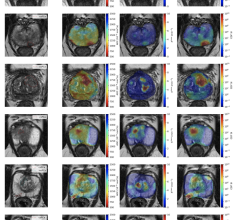
In a smaller subset of patients these clinics have found lingering pericarditis or myocarditis. Most of these patients reported developing chest pain within two week or so after their acute infection. Singh said abnormalities can be imaged using echo and MRI.
"They do typically have abnormalities on imaging. But reassuringly, of all the patients who came to our clinic with these issues, we did not see any decline in left ventricular ejection fraction or systolic function," Singh stressed.
Patients with lingering pericarditis or myocarditis issues are treated with anti-inflammatories. Singh reinforced that the number of patients treated for this have been very low.
"What we do know is that 4 our of 5 patients will have at least one symptom after the acute phase, so this is not a unique thing to be suffering with post-COVID symptoms," Trivax said. "I explain this to patients when they come in, and it is almost as if they are relieved and reassured to hear that they are not alone."
Trivax said the two biggest complaints in post-COVID syndrome patients is fatigue in about 60%, and brain fog in about 30%.
Baggish said cough, chest pain, rapid shallow breathing, heart palpitations and resting tachycardia are the symptoms he has seen in many of his patients. He explained tachycardia is one of the primary cardiac presentations in long-COVID. Another big issue with long-COVID patients tends to be hypervolemia, so it is important to do labs to make sure they are not dehydrated.
Singh said the arrhythmias he has seen include atrial fibrillation (AF) and supraventricular tachycardia. He noted ventricular tachycardia is very rare in these patients. In discussions with his electrophysiology (EP) colleagues, Singh believes the issues with post-COVID arrhythmias often comes down to the substrate of the patient's heart. He said the more cardiovascular disease, cardiomyopathy, scarring, or previous AF a patient has, the more predisposed they are to developing an arrhythmia after a COVID infection.
However, Cedars-Sinai has seen a handful of younger, healthier patients with no history or cardiac problems presenting with arrhythmias as they recovered from COVID. Some had risk factors for developing arrhythmias and it is theorized COVID may bring out these issues in patients. Singh said it is likely these patients would have presented with AF later in life if it was not for catching COVID.
Many of the patients Trivax has seen only had a mild case of COVID, but presenting months later with cardiac issues. Trivax said these patients often test troponin positive. The question as to what is causing this often results in a cardiac MRI.
"There are also patients who had very mild symptoms [during their COVID infection] and those patients don't have a major event, however, they may have those prolonged symptoms," Trivax said. "We see this in the MRI studies that have been performed. But, what these abnormal cardiac MRIs really mean, we don't quite know. We don't have any long-term data for these COVID patients."
It is not clear if there if there might be residual micro-emboli or other causes, such as a lyme disease-like reaction to the virus in the body. "We don't quite know, and that really defines COVID," Trivax said.
Predicting Which Patients Will Get Long-COVID Symptoms
The severity of illness from the acute phase of the COVID infection is the primary predictor for who will likely develop long-COVID symptoms later. But, Baggish said in the clinic, they have at times seen patients who have very mild or even asymptomatic infections come in with long-hauler symptoms, so he explained this can really happen to anyone who has had COVID. However, most long-haulers presenting with clinical symptoms did have a more serious COVID infection, but the prevalence of long-COVID varies across different populations.
Baggish said health, wellness and age of patients have a lot to do with how sick they get during acute infections and issues they experience with long-COVID. He said more than 50% of older patients with significant comorbidities will experience some form of long-COVID. “And this can be very heterogeneous, with any symptom in the body from head to toe,” he said. “We really don’t understand why that happens to some people, but not others.” Baggish said, adding they tend to show symptoms between one and six months from their initial infection.
"In younger, collegiate athletes, where I spend most of my time, we see a very different story. We see a much, much lower provenance of long-COVID, on the order of less than 1%," Baggish explained.
There could be causes rooted in the acute infection that causes several cardiac complications. However most of the worst cardiac related issues are mainly seen in very sick, hospitalized patients. “We know there are acute cardiovascular complications that occur in the acute phase of COVID infection," Trivax said. "These include arrhythmia, myocardial infarction whether it is just demand ischemia or actually a thrombotic event, and then there is the thrombophilia part of it with issues like DVT and pulmonary embolism. There also are issues with myocarditis and pericarditis that might cause long-term damage.”
Long-COVID is Very Similar to POTS
A year ago, post-COVID clinical complaints appeared to be a big concern because there was so much that was unknown. However, it has became clear after studying these patients that this is not such a new condition as originally thought. Trivax said long-COVID is very similar to the autonomic dysfunction caused by postural orthostatic tachycardia syndrome (POTS). He said POTS is a disease clinicians do not like to treat because the patients can be very challenging, but POTS patients, like long-COVID, can be treated.
"From a cardiac standpoint, about 20-40 percent of patients do tend to have features of reminiscent of POTS, or inappropriate sinus tachycardia," Singh said. "We have known about these issues for years, and they have been described after patients had other viral illnesses."
He said they have done standard tilt table studies in these patients to reveal abnormalities in heart rate response. The patients are treated in a similar way as POTS patients would be.
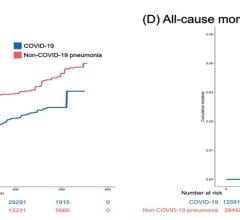
Heart Attacks, Strokes and Heart Failure Are Not Seen in Long-COVID Cases
There was a lot of concern in 2020 that the long-term impact on the heart and blood vessels from COVID infection would result in an increase in heart failure cases and vascular issues involving clotting. Luckily, the experts said this has not been the case.
"We are not seeing new heart attacks, new strokes or heart failure admissions as a function of long COVID," Baggish said. He said the usual cardiac presentations include heart palpitations and chest pain, which generally do not come with any clear findings on diagnostic testing. He said myocarditis is typically part of the acute phase of infection and generally not an issue in the long-COVID cases they have seen at Mass General.
For the small number of cases that do show signs of myocarditis or residual clotting that is usually only seen in acute cases, there is a question if this is truly a result of a previous infection, or due to ongoing viral load.
"As a cardiologist, the main unanswered question I wrestle with is how much of COVID is a function of residual infection which has not been cleared, versus long-term target organ damage. So, if the heart or lung vessels were damaged during COVID, or the symptoms people feel reflect that damage, is there still virus in the body?
"Palpitations are a very common component of long-COVID," Baggish said. "When we do ambulatory rhythm monitoring on these patients we see, for the most part, benign atrial or ventricular atopic beats, so not things that would confer risk, but certainly something that patients can and do feel."
Thrombosis is Very Rare in Long-COVID Patients
Acute COVID is known to cause clots in a significant number of several acute infections. There was a question a year ago if this would continue after the infection and if it was the cause of many long-COVID symptoms. But, this does not appear to be the case.
"When we first started treating COVID patients, I remember being in the intensive care unit and we had an overwhelming sense of shock that patients requiring urgent hemodialysis, they were all clotting their lines off. This was before we were giving patients heparin. We know now that this induces a dramatic thrombophilic like state.
The COVID-caused clotting also occurred throughout the body in the acute phase, leading to strokes, DVT, heart attacks and infarcts in various organs. However, all three experts said they have not seen much in the way of macro clotting after a few weeks out from the acute infections. But, they add there is a possibility of micro emboli in the capillaries being a possible culprit for some of the long-COVID issues that are seen, which would not show up on CT or MRI.
What Tests are Ordered to Evaluate Cardiac Long-COVID Patients?
Cardiac patients at the Cedar-Sinai long-COVID clinic are evaluated with a basic physical exam, extensive family and medical history, an ECG, basic labs that include troponin and BNP, D-dimer, A1C, lipid panel and a metabolic profile since many patients have become much less active during the pandemic. Patients with symptoms are evaluated with an echocardiogram, including global longitudinal strain. If patients have abnormalities on the echo, or if there is suspected pericarditis or myocarditis, the patient is referred for a cardiac MRI with contrast.
Trivax said the small number of patients presenting to the clinic with myocarditis symptoms go through a battery of tests to exclude other major pathology issues. He recommends an echocardiogram, ECG, troponin and an ambulatory monitor to check for any arrhythmias.
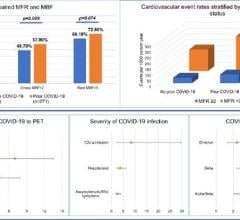
Cardiac MRI Is Not Showing Long-term Myocardial Damage
In 2020, an MRI study came out of Europe that showed myocardial damage in a high number of COVID patients. However, more than a year later, Singh said this damage is not being seen seen in MRIs of long-haulers. Instead, it is very likely cardiac edema was mistaken for damage, and that is seen on many cardiac MRIs but does not mean there is any damage to the heart.
Singh divides the clinic patient populations into two groups, those with mild cases of COVID managed at home, and patients who were hospitalized with more severe acute infections. He said most of the clinic patients they see had mild or asymptomatic infections.
"For the most part, we are not seeing major abnormalities in MRI," Singh explained. "Even in the patients who had pericarditis, the left ventricular function was normal."
In patients who had been critically ill, that is where we some signal for cardiac damage," he said, explaining these were the patients in the ICU with severe respiratory failure. It is rare, but they have found evidence of severe cardiac disfunction in some of these patients.
He said this is especially true in patients whose ejection fractions were very low during their acute infections. MRIs from discharge and later followups have shown abnormalities such as cardiac edema, abnormal T1 and T2 times and late gadolinium enhancement. But, he adds these patients have been fairly easy to treat. He said larger doses of steroids during the acute phase, and then with vasodilators after they start to recover and blood pressure returns to normal, and they have seen improvement and normalization in ejection fractions.
Singh said a few of these patients have been followed out for more than 6 months, and none showed signs of decline in cardiac function, which was the big fear in late 2020.
There have been numerous post-COVID cardiac MRI studies over the past two years and a key takeaway is that not everyone needs a cardiac MRI. Also, MRI might be over utilized right now for long-COVID evaluation.
Evaluation of Long-COVID in Student Athletes
There also have been questions about the use of MRI to screen student athletes for post-COVID cardiac inflammation.
"The use of MRI to screen athletes has been an incredibly controversial topic that is still somewhat unresolved," explained Baggish. "I will tell you that there are now multiple guidelines in place, many of which I have either written or co-authored, that make a very important point that using the MRI to screen for heart inflammation is a bad idea. We simply are not at a point where MR should be used as a screening tool. Where it has been used for this, it has led to more confusion and questions than it has answered."
He said it can lead to over diagnosis. There are technical issues that vary from one MRI scanner to another so there is a lack of normative data, cost and discomfort make MRIs problematic.
"For athletes, it boils down to their level of acute illness. That includes people who had cardiac symptoms in their acute illness, so that means chest pain, unusual shortness of breath, exercise intolerance, arrhythmias — those make up the minority of patients, but those are the ones we care about," Baggish said.
He said the standard of care diagnosis in these patients is usually the triad test, which includes ECG, echo and troponin, and they use the results from that to determine if further testing is needed.
Do Not Tell Patients Long-COVID Symptoms are All in Their Head
About 75% of patients with long-hauler symptoms have been told their issues are not long-COVID related, and the symptoms are psychosomatic, or that they are experiencing depression, but there is just so much more to it than that, Trivax explained. He said clinicians need to take patients seriously when they complain about what appear to be long-COVID symptoms.
Singh said Cedars-Sinai has psychologists involved in their long-COVID clinic to help address patients who have depression, and after exhausting testing options that do not reveal any pathological reason for their complaints.
"It really has to be the end after a long thoughtful process with the right diagnostics to implicate the the mind as being the cause of all this. The last thing in the world that will be helpful in the clinical suite is to tell a patient they are imagining these things. That is the surest way to never see a patient again," Baggish said.
Vaccinations Have Helped Prevent Large Numbers of Acute Cases With Related Long-COVID Problems
Vaccinations over the past year have helped greatly reduce the number of patients with cardiac or other comorbidities from getting severe COVID infections, Singh said. Cardiac patients and anyone with comorbidities that can magnify the impact of COVID infections were among the first patients prioritized for the vaccine in early 2021. Sign said this has had a big impact on lowering the number of these patients ending up in hospitals with severe COVID cases. He said this has helped blunt the expected tidal wave of cardiac long-hauler COVID patients who were already unhealthy prior to the pandemic.
He urges all his long-COVID patients to get vaccinated or boosted if they have not already. He said that will go a long way to preventing future infections and possibly worse outcomes if they get infected again.
When Will Medicine Have All the Answers on Long-COVID?
While there is much more known today about long-COVID than a year ago, the root causes of some of the common post-COVID complaints still have not been completely answered.
"I think it will take more than a year, because with each new variant that comes through causes different types of acute infection profiles and probably have different long-COVID implications," Baggish said. "We are just now figuring out the implications of the alpha and beta variants, and we will need more time to figure out delta and omicron. We need time to figure out the pathophysiology, and it will take even longer to find out if there are any hard outcomes that matter with respect to mortality, morbidity and infirmity. This will take about four to five years to really understand."
Related Long-COVID Content:
VIDEO: Long-COVID Presentations in Cardiology at Beaumont Hospital — Interview with Justin Trivax, M.D.
VIDEO: Long-term Cardiac Impacts of COVID-19 Two Years Into The Pandemic — Interview with Aaron Baggish, M.D.
The Long-term Cardiovascular Impact of COVID-19 (Jan. 2021 article)
VIDEO: What Are The Long-term Cardiac Impacts of COVID-19 Infection — Interview with Todd Hurst, M.D.
VIDEO: Lingering Myocardial Involvement After COVID-19 Infection — Interview with Aaron Baggish, M.D. (2020)
Find more COVID news and video

 March 20, 2024
March 20, 2024