July 1, 2010 – The U.S. Food and Drug Administration (FDA) recently added a warning to the information on clopidogrel (Plavix), as a result of new information indicating that variations in genetic makeup can prevent the medication from reducing patients’ risk for heart attack and stroke. To help clinicians interpret the new FDA warning for this widely prescribed antiplatelet agent, the American College of Cardiology Foundation (ACCF) and the American Heart Association (AHA) released a joint clinical alert, shedding light on key issues for consideration and recommendations for practice.
“Just as some people have red hair and others have blonde, our genetic makeup can also affect the way we respond to certain drugs, such as clopidogrel,” said David Holmes Jr., M.D., chair of the six-member writing group. “The majority of patients do very well with standard guideline-based clopidogrel, but for the small number of patients who have problems, these are big problems.”
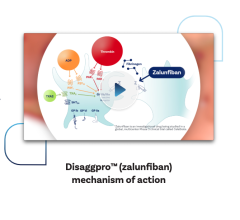
Drugs like clopidogrel work by making platelets less likely to form blood clots, and have been shown to lower the risk of heart attack, unstable angina (new or increased heart pain), stroke and heart-related death in patients. However, because antiplatelet effects don’t occur unless the body converts or metabolizes the drug into its active form, patients with certain differences in their genetic makeup will not derive clinical benefit and, instead, remain at risk for serious adverse events. The FDA estimates that two to 14 percent of patients are “poor metabolizers” of the drug, thereby not benefiting fully from it.
The report reviews the backdrop for the new prescribing information, including the multiple unknown factors that can influence individual patient outcomes. It also sets forth broad recommendations for practice:
• Adherence to existing evidence-based guidelines from ACCF, AHA or other professional societies for using antiplatelet therapies should remain the foundation of care. If clopidogrel is prescribed, health care providers should help ensure that patients take it as prescribed.
• Clinicians must be aware that in certain patients with either acute or chronic coronary artery disease, genetic variability in response to clopidogrel can affect its inhibition of platelet function.
• Careful clinical judgment, including weighing the risks and benefits, is needed in considering all therapies. The new boxed warning points out that for clopidogrel, if there is a lack of efficacy, the consequences can potentially result in fatal outcomes.
• Results from ongoing clinical trials in large groups of patients will provide more information about the predictive value of genetic testing and better inform the role genotyping might play in personalizing medicine and optimizing outcomes.
• Genetic testing to determine if a patient is a “poor metabolizer” may be considered before starting clopidogrel therapy in patients believed to be at moderate or high risk for poor outcomes (e.g., patients undergoing elective high-risk percutaneous coronary interventions).
• Using alternative antiplatelet therapies or altering the dosing of clopidogrel may be reasonable options in patients who experience an adverse event while taking clopidogrel and have been taking the drug as prescribed.
Authors caution that patients currently taking clopidogrel should not stop the drug unless advised by their health care provider.
The American Academy of Family Physicians, Society for Cardiovascular Angiography and Interventions and the Society for Thoracic Surgeons have also endorsed the recommendations presented in the ACCF/AHA advisory.
For more information: www.cardiosource.org


 January 28, 2026
January 28, 2026