Photo credit: Getty Images
October 31, 2022 — Results from the Late-Breaking Clinical Trials session at The VEINS Conference in Las Vegas, NV, were announced on Oct. 31 by the VIVA Foundation, a not-for-profit organization dedicated to advancing the field of vascular medicine and intervention through education and research. The VEINS (Venous Endovascular INterventional Strategies) is an annual venous education symposium where global, multispecialty faculty to present a comprehensive variety of talks and case presentations focused on venous care.
Highlights follow on the six late-breaking clinical trial presentations as released by the organization:
- In-Hospital and 30-Day Outcomes from the Fully Enrolled, Multicenter, Prospective CLOUT Registry;
- ABRE Study: Clinical Outcomes by Initial Clinical Presentation through 36 Months;
- Propensity Score–Matched Analysis of Early Clinical Outcomes from the CLOUT and ATTRACT Studies;
- Single-Session Thrombectomy for the Treatment of Iliofemoral Deep Venous Thrombosis (DVT) Is Associated with Reduced ICU Cost When Compared With Thrombolysis;
- First-in-Human Study Results with Amplifi Vein Dilation System Treatment;
- Improvement in Clinical and Echo Parameters After Computer-Aided Mechanical Aspiration Thrombectomy for Treatment of Acute Pulmonary Embolism
“In-Hospital and 30-Day Outcomes from the Fully Enrolled, Multicenter, Prospective CLOUT Registry” was presented by David Dexter, MD. The CLOUT (ClotTriever Outcomes) registry is an all-comer, multicenter study evaluating patient outcomes following treatment of proximal, lower extremity deep vein thrombosis (DVT) with the ClotTriever System (Inari Medical). This analysis from the now fully-enrolled registry represents the largest mechanical thrombectomy study in the field of DVT. All-comer patients were enrolled — irrespective of symptom duration, thrombus age, prior failed treatment of the current DVT, or bilateral disease — providing a generalizable patient population.
The primary endpoint was complete or near-complete (≥ 75%) thrombus removal, assessed by an independent core laboratory. The primary endpoint was achieved in 91.2% of limbs, and the 30-day device-related SAE rate was 0.2%. Nearly all procedures were single session (99.4%), median estimated blood loss was low (40.0 mL), and only 2.2% of patients received overnight post-thrombectomy intensive care unit monitoring. Patient symptoms (eg, pain and edema) were significantly reduced at discharge and showed sustained improvement through 30 days.
Further significant 30-day outcomes include recovery of vessel flow and compressibility as measured by duplex ultrasound, improvements in revised Venous Clinical Severity Score and EuroQoL five dimensions quality-of-life score, median 5.5-point reduction in Villalta score, and < 10% of patients with a moderate or severe Villalta score (≥ 10).
This analysis of the CLOUT registry, according to researchers, shows the excellent safety profile and effective thrombus removal of mechanical thrombectomy with the ClotTriever system in a real-world DVT patient population.
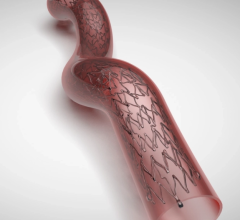
The “ABRE Study: Clinical Outcomes by Initial Clinical Presentation Through 36 Months,” was presented by Stephen A. Black, MD. This study is a prospective, interventional, multicenter study that evaluated 200 participants with symptomatic iliofemoral venous outflow obstruction. Participants were categorized based on initial clinical presentation by the enrolling investigator as postthrombotic syndrome (PTS) (47.5%), nonthrombotic iliac vein lesion (NIVL) (36.0%), or acute (posttreatment) deep vein thrombosis (aDVT) (16.5%).
The long-term primary endpoint was freedom from target lesion revascularization (TLR) at 36 months. Long-term secondary endpoints included primary patency, freedom from clinically driven TLR, delayed stent migration, stent fracture, quality-of-life (QOL) measures, and venous functional assessments through 36 months. Based on Kaplan-Meier estimate, the 3-year primary patency rate was 70.4%, 97.1%, and 76.5% for PTS, NIVL, and aDVT, respectively. The mean Villalta score in the target limb and mean Venous Clinical Severity Score decreased from baseline to 36 months for all initial clinical presentations.
The 3-year outcomes of the ABRE study support the safety and effectiveness of the Abre venous self-expanding stent (Medtronic) when used to treat symptomatic iliofemoral venous outflow obstruction across all initial clinical presentations. Participants who received an Abre venous stent reported clinically significant improvement in QOL and functional outcome measures through 3 years when compared to baseline.
“Propensity Score–Matched Analysis of Early Clinical Outcomes From the CLOUT and ATTRACT Studies,” presented by Steven Abramowitz, MD, was a reference trial evaluating interventional treatment for deep vein thrombosis (DVT). Researchers reported that it no added benefit compared to anticoagulation, noting that new interventions have emerged since the completion of ATTRACT, and their comparative effectiveness is unknown. Using propensity score–matched data, the team compared outcomes from the largest mechanical thrombectomy study, the CLOUT registry, with those from the ATTRACT trial.
To adjust for differences in study design, patients with bilateral DVT, symptom duration > 4 weeks, or incomplete case data were excluded. Propensity score matching (1:1) on 11 baseline covariates (age, sex, body mass index, sidedness, prior VTE, race, symptom duration, DVT location, presence of provoked DVT, Villalta score, and Marder score) was performed between the remaining CLOUT and ATTRACT patients, resulting in 166 matched pairs.
No significant differences in baseline characteristics remained after matching. Rates of stenting and venoplasty were similar between the groups and, as expected based on differences in mechanism of action, rates of thrombolytic use and postprocedural hospital overnights were significantly different.
Further, noted the author, thrombus extraction as measured by core laboratory–assessed Marder scores was 22.3% better in CLOUT patients (P < .0001), and 22.2% more CLOUT patients achieved ≥ 75% thrombus clearance (P < .0001). Similarly, 12.7% fewer CLOUT patients had Villalta scores ≥ 5 at 30 days (P < .05). Logistic regression on ATTRACT showed that 30-day Villalta scores significantly predicted PTS at 6 months, 1 year, and 2 years, highlighting the potential long-term effect of these differences.
In this propensity score–matched analysis, CLOUT patients showed better thrombus extraction and improvement in 30-day Villalta scores than ATTRACT patients. Thirty-day Villalta scores in ATTRACT predicted PTS through 2 years, suggesting potentially long-term implications for these findings. Future randomized controlled trials, such as DEFIANCE, will further clarify the role of the ClotTriever system (Inari Medical) in treating DVT, the authors noted.
“Single-Session Thrombectomy for the Treatment of Iliofemoral Deep Venous Thrombosis (DVT) Is Associated with Reduced ICU Cost When Compared with Thrombolysis,” presented by John Filtes, MD, was also one of the first late-breaking trials reported.
The authors noted that lower extremity deep vein thrombosis (DVT) is a major cause of morbidity in the United States, with significant associated health care costs. For iliofemoral DVT, catheter-directed therapies lead to reduction in venous hypertension and inflammatory response to the acute thrombus, thereby reducing clinically significant chronic venous insufficiency, also known as postthrombotic syndrome. Mechanical thrombectomy devices have recently been developed that remove the thrombus using a combination of suction techniques—without the need for thrombolytics—and allow for stenting in a single session.
In this retrospective review of all patients who underwent thrombectomy and thrombolysis for the treatment of iliofemoral DVT (at two large medical centers in the 10-year period from 2011 to 2021), researchers sought to compare costs of postprocedural intensive care for patients treated with single-session mechanical thrombectomy versus thrombolysis for DVT (often double-session). Thrombolysis was associated with approximately $6,000 of additional intensive care costs compared with single-session thrombectomy. Also, thrombolysis incurred the additional cost of thrombolytics, which were not used for thrombectomy. The research team noted that future studies will aim to analyze total health care costs associated with treatment of DVT, inclusive of ICU, procedure, and physician costs.
Results from the “First-in-Human Study Results With Amplifi Vein Dilation System Treatment,” were presented by Surendra Shenoy, MD, PhD. It was noted that three million patients worldwide with end-stage renal disease (ESRD) need reliable vascular access for hemodialysis. A forearm arteriovenous fistula (AVF) that has fewer complications and preserves proximal sites for future access is the best initial access option. However, maturation failure of forearm AVF is as high as 85% and only 32% of AVFs are attempted in the forearm. Small vein diameter strongly correlates with maturation failure; 6-mm veins have a 75% probability of maturation versus 10% for 3-mm veins.
The Amplifi vein dilation system (Artio Medical, Inc.) comprises a wearable pump and catheters that help dilate veins prior to AVF creation. The Amplifi system delivers nonpulsatile, supraphysiologic wall shear stresses within the target vein to stimulate flow-mediated dilation. The treatment yields dilated veins that have a higher probability of maturation with subsequent AVF creation.
The first cohort of five ESRD patients in a prospective, nonrandomized, single-arm, open-label, first-in-human clinical study were treated at Sanatorio Italiano in Asunción, Paraguay, between Q1 and Q3 2021. A second cohort was treated in Q3 2022. Mean treatment duration was 8.6 days in cohort 1 and 6.3 days in cohort 2. All AVFs in cohort 2 were created in the forearm. After treatment, an AVF was created with a treated vein, and ultrasound examination was performed at day 1, week 2, and week 6. Treatment with the Amplifi system resulted in a 151% increase in cephalic vein diameter, with a 134% concomitant increase in flow rate. AVFs made with treated veins were fully mature within 2 weeks, and all patients were cleared for hemodialysis using their AVFs by week 6. The presented noted that the Amplifi system is in development and not available for commercial use.
Findings of the “Improvement in Clinical and Echo Parameters After Computer-Aided Mechanical Aspiration Thrombectomy for Treatment of Acute Pulmonary Embolism,” trial were presented by Elias Iliadis, MD.
Changes in clinical findings after treatment of acute pulmonary embolism (PE) with mechanical aspiration thrombectomy may lend insight into the timing of recovery from the index event. In published studies of PE patients, right heart function can be evaluated by echocardiography and provide additional measures of right heart function. The purpose of this study was to evaluate improvement in clinical and echocardiographic parameters after treating acute PE patients with computer-aided mechanical aspiration thrombectomy with the Indigo Lightning 12 aspiration system (Penumbra, Inc.).
This single-center, retrospective review included patients undergoing treatment for acute PE with Lightning 12 aspiration thrombectomy (August 2020 and February 2022). Clinical and echocardiographic parameters were assessed preprocedure and 48 hours post-procedure.
Sixty-three patients were treated. Most had submassive PE (83%), and 97% were bilateral. Posttreatment, there was significant reduction in clinical variables of heart rate (73% vs 8%), episodes of hypotension (27% vs 3%), hypoxia (16% vs 0%), and Pulmonary Embolism Severity Index scores (117 vs 83). There was improvement in echocardiographic parameters, including pulmonary artery (PA) pressure, median right ventricular/left ventricular ratio, PA compliance, median acceleration time, and median tricuspid annular plane systolic excursion. Average thrombectomy time was 18 minutes, and estimated blood loss was 381 mL.
Treatment of acute PE with computer-aided mechanical aspiration thrombectomy resulted in rapid improvement of vital signs and right heart function, as measured by echocardiography. This was accomplished with a short procedure time and an acceptable safety profile.
More information: https://thevivafoundation.org
Related Content:
Late-breaking Clinical Trial presentations announced for The VEINS and VIVA Conference


 November 09, 2025
November 09, 2025