Photo credit: The VIVA Foundation
November 2, 2022 — The second round of late-breaking clinical trial results were announced at VIVA22 on Nov. 1 in Las Vegas, NV. The VIVA Foundation is a not-for-profit organization dedicated to advancing the field of vascular medicine and intervention through education and research and coordinates VIVA (Vascular InterVentional Advances), an annual vascular education symposium. The event, which followed THE VEINS Conference, held Oct. 30-31, brings together a global, multispecialty faculty to present a variety of talks and live case presentations from clinical centers around the world. Below are summaries of this second set of late-breaking clinical trial presentations, which included:
- Three-Year Results of the GORE VIABAHN Stent Graft in the Superficial Femoral Artery for In-Stent Restenosis
- Cross-Seal IDE Trial: Prospective, Multi-Center, Single-Arm Study of the Cross-Seal Suture-Mediated Vascular Closure Device System
- Periprocedural and Patient-Reported Quality of Life Outcomes After Computer-Aided Mechanical Aspiration Thrombectomy for the Treatment of Acute Pulmonary Embolism: Interim Analysis of the STRIKE-PE Study
- Safety and Performance of the Indigo Aspiration System for the Treatment of Lower Extremity Acute Limb Ischemia: Interim Analysis of the STRIDE Study
- Twelve-Month Results From a Prospective Study of the Rotarex Atherectomy and Thrombectomy Catheter System
- 6-Month Results from the PROMISE II US Pivotal Trial of the LimFlow System
“Three-Year Results of the GORE VIABAHN Stent Graft in the Superficial Femoral Artery for In-Stent Restenosis,” was presented by Peter A. Soukas, MD. The RELINE MAX study is the first report of long-term, 36-month outcomes of the postmarket approval study of the Gore VIABAHN endoprosthesis (Gore & Associates) for the treatment of bare-metal in-stent restenosis (ISR) in the superficial femoral artery (SFA).
RELINE MAX was a prospective, single-arm international study that enrolled patients at 23 sites from October 2015 to April 2018. Patients with ≥ 50% ISR or occlusion in the SFA, Rutherford category 2-5 disease, and ≥ 1 patent runoff vessel were eligible. The primary effectiveness endpoint was primary patency at 12 months. The primary safety endpoint was rate of device- or procedure-related serious adverse events (SAEs) at 30 days.
A total of 108 patients were enrolled in the study; 86 were included for analysis through 3 years (mean age, 70.9 ± 10.4 years; 48.8% female). Mean core lab–reported lesion length was 12.4 ± 6.92 cm (29.1% occluded lesions); 10.5% of patients presented with chronic limb-threatening ischemia and 81.9% of lesions were Tosaka class II and III. Acute procedural success was 98.8%. Freedom from device- or procedure-related SAEs was 96.5% through 30 days. At 1 year, primary, primary-assisted, and secondary patency rates were 74.7%, 80.4%, and 89.4%, respectively. Freedom from target lesion revascularization was 84.8%, 74.6%, and 65.0% at 1, 2, and 3 years, respectively. Per core lab assessment, no major amputations or device fractures occurred through 3 years. At 3 years, 80.4% of patients had ≥ 1 Rutherford category improvement.
More recent studies from Japan using the study device in de novo SFA lesions suggest high primary patency rates with use of intravascular ultrasound (IVUS) to avoid oversizing the device by 20%. A prospective evaluation of stent grafting for the treatment of femoropopliteal ISR utilizing IVUS and best practices is needed to improve the long-term outcomes of patients with long, complex femoropopliteal ISR.
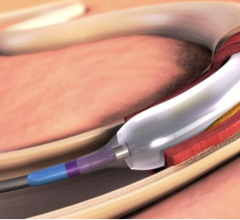
“Cross-Seal IDE Trial: Prospective, Multi-Center, Single-Arm Study of the Cross-Seal Suture-Mediated Vascular Closure Device System” findings were shared by Prakash Krishnan, MD. The objective of this prospective, multicenter, single-arm trial (NCT03756558) was to determine the effectiveness and safety of the Cross-Seal suture-mediated vascular closure device (VCD; Terumo Interventional Systems) in obtaining hemostasis at the target limb access site after interventional procedures using 8- to 18-F procedural sheaths.
The trial included patients undergoing transcatheter aortic valve replacement (TAVR), balloon aortic valvuloplasty, or endovascular thoracic or infrarenal aortic aneurysm repair (TEVAR/EVAR) using 8- to 18-F sheath sizes. The primary efficacy endpoint was time to hemostasis (TTH) at the target limb access site, and the primary safety endpoint was freedom from major complications of the target limb access site within 30 days.
A total of 147 patients were enrolled between August 9, 2019, and March 12, 2020. TAVR was performed in 53.7% (79/147) and percutaneous TEVAR/EVAR in 46.3% (68/147). The mean sheath inner diameter was 15.5 ± 1.8 mm. The primary effectiveness endpoint of TTH was 0.4 ± 1.4 minutes; the median was 0.05 minutes (IQR, 0.017-0.15 minutes). Adjunctive intervention was required in 9.2% (13/142), of which 2.1 (3/142) were surgical and 5.6% (8/142) endovascular. Technical success was achieved in 92.3% (131/142) of subjects. Freedom from major complications of the target limb access site was 94.3% (83/88).
Results of the study “Periprocedural and Patient-Reported Quality of Life Outcomes After Computer-Aided Mechanical Aspiration Thrombectomy for the Treatment of Acute Pulmonary Embolism: Interim Analysis of the STRIKE-PE Study” were offered by Ido Weinberg, MD.
The objective of the STRIKE-PE study is to evaluate real-world safety, performance, and functional outcomes of computer-aided mechanical aspiration thrombectomy with the Indigo Lightning 12 aspiration system (Penumbra, Inc.) for the treatment of pulmonary embolism (PE). This summary reports the periprocedural and patient-reported quality-of-life outcomes from an interim analysis of the study.
STRIKE-PE is a prospective, multicenter study of adult patients with clinical symptoms consistent with acute PE of ≤ 14 days and right ventricular/left ventricular (RV/LV) ratio ≥ 0.9 who received frontline endovascular treatment with Lightning 12.
This interim analysis included 60 patients. The mean patient age was 59.4 years, 43.3% were female, and 95.0% had submassive PE. Of the patients with an intensive care unit (ICU) stay, the median ICU length of stay was 1 day; 34.5% (19/55) did not require an ICU stay. The median improvement in RV/LV ratio from baseline to 48 hours was 0.27 (P < .001)—a reduction of 24.3%. The mean improvement in systolic pulmonary artery pressure (sPAP) from before to after thrombectomy was 10.6 mm Hg (P < .001)—a reduction of 19.9%.
Treating acute PE with computer-aided mechanical aspiration thrombectomy with Lightning 12 resulted in periprocedural reduction in RV/LV ratio and sPAP, as well as improvement of patient-reported quality of life at 90-day follow-up.
“Safety and Performance of the Indigo Aspiration System for the Treatment of Lower Extremity Acute Limb Ischemia: Interim Analysis of the STRIDE Study,” was presented on Nov. 1 by Thomas Maldonado, MD.
This interim analysis reports safety and performance data from STRIDE to evaluate the benefits of aspiration thrombectomy for patients with lower extremity acute limb ischemia (LE-ALI). STRIDE is a global, prospective, multicenter study, enrolling up to 130 participants presenting with LE-ALI. Participants were treated with frontline aspiration thrombectomy using Indigo aspiration (Penumbra, Inc.) prior to stenting or angioplasty.
The primary endpoint is the target limb salvage rate at 30 days post procedure. Secondary endpoints include technical success, as defined by core lab–adjudicated thrombolysis in myocardial infarction (TIMI) 2/3 flow rate immediately post procedure, and change in modified Society for Vascular Surgery (SVS) runoff score.
Of 96 participants enrolled from 14 sites, the mean age was 65.9 years (46.9% female). Ischemic severity at baseline (n = 95) was classified as Rutherford class 1 in 5.3% of patients, Rutherford class 2a in 57.9% of patients, and Rutherford class 2b in 36.8% of patients. Mean thrombus length was 109.9 ± 115.8 mm. Prior to the procedure, 94.5% of patients (69/73) had no flow (TIMI 0) through the target lesion. The most common thrombus location was the popliteal in 66.0% of patients (62/94), followed by the superficial femoral in 44.7% (42/94).
The target limb salvage rate at 30 days was 97.9% (94/96). The rate of periprocedural major bleeding was 4.2%, and device-related serious adverse events was 1.0%. Flow restoration (TIMI 2/3) was achieved in 94.4% (67/71) of patients immediately post procedure. Median improvement of modified SVS runoff score (after vs before procedure) was 5.0 (0.0, 10.0).
In this interim analysis, STRIDE patients treated with Indigo aspiration had low 30-day amputation rates, low periprocedural complications, and high rates of technical success.
Mechanical aspiration thrombectomy provided an effective endovascular treatment option in this population of LE-ALI patients.
“Twelve-Month Results from a Prospective Study of the Rotarex Atherectomy and Thrombectomy Catheter System,” presented by Michael Lichtenberg, MD, was a prospective, multicenter, single-arm study; it was designed to assess the technical/procedural success, safety, and primary patency of the Rotarex catheter (BD Interventional), a rotating and aspirating atherectomy and thrombectomy catheter system. A total of 220 patients were enrolled at 14 centers in Europe from July 2019 through September 2020. Ethics approval and informed consent were obtained prior to enrollment in the study.
The technical/procedural success, defined as the ability to cross and successfully treat the target lesion, was measured at completion of the index procedure. The safety measure, defined as freedom from major adverse events (MAEs), was collected through 30 days. Primary patency was collected at 1, 6, 12, and 24 months and defined as freedom from clinically driven target lesion revascularization (TLR) and freedom from > 50% stenosis (peak systolic velocity ratio < 2.5). Secondary outcomes at 1, 6, 12, and 24 months included safety events, freedom from target vessel revascularization (TVR), walking improvement (VascuQoL-6), quality-of-life improvement (EQ-5D-3L), and various subcohort analyses.
Freedom from MAEs through 30 days was 94.4%. Technical/procedural success where Rotarex was used alone was 47.2%. When used with adjunctive treatments (in 97.7% of the cohort), technical/procedural success was 94.1%. Primary patency at 1, 6, and 12 months was 87.2%, 68.1%, and 57.8%, respectively. Freedom from TLR at 1 month was 96.7%, and freedom from TVR at 1 month was 99.1%; these were sustained through 6 and 12 months. Most patients showed improvement in Rutherford class, and improvements were also observed in the quality-of-life measures.
Results showed a freedom from MAE rate of 94.9% at 1 month. Technical/procedural success with adjunctive treatments was 94.1%, with a primary patency rate of 57.8% at 12 months. The Rotarex catheter study is an ongoing study with a follow-up period of 24 months.
“6-Month Results from the PROMISE II US Pivotal Trial of the LimFlow System,” was presented by Daniel Clair, MD. PROMISE II is a pivotal trial of the LimFlow system for transcatheter arterialization of the deep veins (TADV) (LimFlow, Inc.). The trial was a multisite, single-arm, prospective study designed with a composite primary endpoint of amputation-free survival (AFS). The study included patients with chronic limb-threatening ischemia who were felt to have no option for arterial revascularization into the foot. The lack of option was confirmed by an independent review committee of vascular surgeons.
The trial enrolled 105 patients with a mean age of 69 years, 69% of whom were male. Over 75% of patients were diabetic, and 18% had end-stage renal disease and were on dialysis. The primary endpoint was compared to a performance goal of 54% AFS based on an extensive literature search for outcomes in this complex group of patients.
Technical success for the procedure in the entire group was 99%, with the majority of procedures being performed to the posterior tibial vessels (75%) and the others connecting the peroneal or tibioperoneal trunk vessels. AFS for the entire group at 6 months was 66%, which was well above the previously identified performance goal, and limb salvage was 76%. More than 75% of wounds were either healed or healing at 6 months, and Rutherford class and pain scores improved over 6 months.
There was a large difference in outcomes for dialysis versus nondialysis patients, which was driven primarily by the increased mortality in the dialysis group. AFS in the nondialysis group was 75%, while AFS in the dialysis group was 37%. Overall survival in nondialysis patients at 6 months was 95%, while survival in the dialysis population was only 63%.
The outcomes for these “no-option” patients were similar to what has previously been published with this technique, and this study showed that the results for TADV with the LimFlow system are better than expected and reproducible, and that this patient population can significantly benefit from this procedure.
For more information: https://thevivafoundation.org
Related content:
https://www.dicardiology.com/content/clinical-trials-venous-care-presented-veins-2022
https://www.dicardiology.com/content/veinsviva-2022-top-awards-recognize-leaders-vascular-medicine


 November 09, 2025
November 09, 2025