Eduardo Marbn, M.D., Ph.D., director of the Cedars-Sinai Heart Institute
June 30, 2009 - Doctors at the Cedars-Sinai Heart Institute said today they completed the first procedure in which a patient's own heart tissue was used to grow specialized heart stem cells that were then injected back into the patient's heart in an effort to repair and regrow healthy muscle in a heart that had been injured by a heart attack.
The minimally-invasive procedure was completed on the first patient June 26.
The procedure is part of a phase I investigative study approved by the FDA and supported by the Specialized Centers for Cell-based Therapies at the National Heart, Lung, and Blood Institute and the Donald W. Reynolds Foundation. It is the first to use adult cells from a patient's own heart to attempt to heal a myocardial infarction.
"This procedure signals a new and exciting era in the understanding and treatment of heart disease," said Eduardo Marban, M.D., Ph.D., director of the Cedars-Sinai Heart Institute, who developed the technique and is leading the clinical trial. "Five years ago, we didn't even know the heart had its own distinct type of stem cells. Now we are exploring how to harness such stem cells to help patients heal their own damaged hearts."
The study is directed by the Cedars-Sinai Heart Institute, with the collaboration of the Johns Hopkins University, where Dr. Marban worked prior to joining Cedars-Sinai in 2007. The 24 patients participating in the study have hearts that were damaged and scarred by heart attacks. Once enrolled in the study, patients go through a three-step procedure.
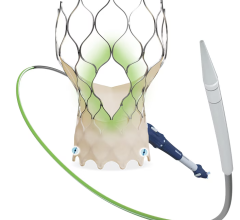
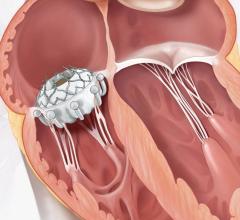
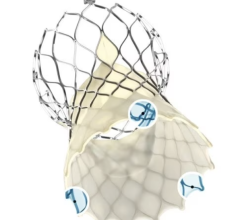
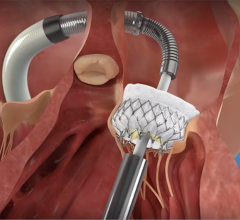
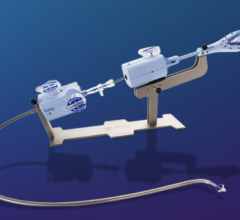
After undergoing extensive imaging so doctors can pinpoint the exact location and severity of the infarction, the patient undergoes a minimally-invasive biopsy, with local anesthesia. Using a catheter inserted through a vein in the patient's neck, doctors remove a small piece of heart tissue, about half the size of a raisin.
The heart tissue is then taken to a specialized lab at Cedars-Sinai, where heart stem cells are cultured using methods invented by Dr. Marban and his team. It takes about four weeks for the cells to multiply to numbers sufficient for therapeutic use, approximately 10 to 25 million.
In the third and final step, the now-multiplied stem cells are reintroduced into the patient's coronary arteries during a second catheter procedure.
All patients in the study had to have experienced heart attacks within four weeks prior to enrolling in the research project. Four patients will receive 12.5 million stem cells and two patients will serve as controls. Later this summer, it is anticipated that 12 more patients will undergo procedures to receive 25 million stem cells, while six additional patients will be monitored as controls.
The first patient, Kenneth Milles, a 39-year-old controller for a small construction company in the San Fernando Valley, experienced a heart attack on May 10 due to a 99 percent blockage in the left anterior descending artery. Milles' heart attack left 21 percent of his heart muscle infarcted. He underwent his biopsy May 24 and received his infusion of stem cells on June 29.
The patients will be monitored for six months. Complete results are scheduled to be available in late-2010.
Dr. Marban, who holds the Mark Siegel Family Foundation chair at the Cedars-Sinai Heart Institute and directs Cedars-Sinai's Board of Governors Heart Stem Cell Center, also said the cardiac stem cell procedure is a logical step forward from recent studies in which cardiac patients have been treated with stem cells derived from bone marrow. Studies over the past eight years have shown that more than 500 cardiac patients have experienced modest improvement when treated with bone marrow stem cells.
However, bone marrow stem cells are not predestined to regenerate heart muscle. When cardiac stem cells were discovered five years ago by various teams worldwide, Dr. Marban began developing a method for isolating heart stem cells from minimally-invasive biopsies and then multiplying the cells. Unlike bone marrow cells, heart stem cells are naturally programmed to regrow heart tissue, so they could prove more effective in healing the injury caused by heart attacks.
"If successful, we hope the procedure could be widely available in a few years and could be more broadly applied to cardiac patients," Dr. Marban said. For example, if patients are able to re-grow damaged heart muscle via stem cell therapy, there could be lesser demand for expensive and risky treatments such as heart transplants.
The process to grow the cardiac-derived stem cells involved in the study was developed by Dr. Marban when he was on the faculty of Johns Hopkins University. The university has filed for a patent on that intellectual property, and has licensed it to a company in which Dr. Marban has a financial interest. No funds from that company were used to support the clinical study. All funding was derived from the National Institutes of Health, the Donald W. Reynolds Foundation and Cedars-Sinai Medical Center.
For more information: www.cedars-sinai.edu


 July 08, 2024
July 08, 2024