May 20, 2013 — If someone suffers a heart attack while walking down the street and is taken to the hospital quickly, his/her chances of survival are very good. But if someone has a heart attack while already in the hospital for something else, he/she is 10 times more likely to die.
That surprising finding comes from a clinical study by University of North Carolina School of Medicine researchers. Their study, which is the first to systematically examine outcomes among hospital inpatients who suffer a type of heart attack called an ST elevation myocardial infarction (STEMI), was published in April in the Journal of the American Heart Association.
“We found that the survival rate for outpatients brought to UNC Hospitals for STEMI treatment was slightly more than 96 percent,” said George A. Stouffer, M.D., distinguished professor in the UNC School of Medicine and senior author of the study. “But the survival rate for inpatients who suffered a STEMI was much lower, only 60 percent.”
Part of the difference is explained by the fact people who suffer a STEMI while hospitalized are, as a group, older and sicker than people who suffer a STEMI outside the hospital. But even after adjusting the statistical analysis to account for this, there were still important differences in survival, Stouffer said.
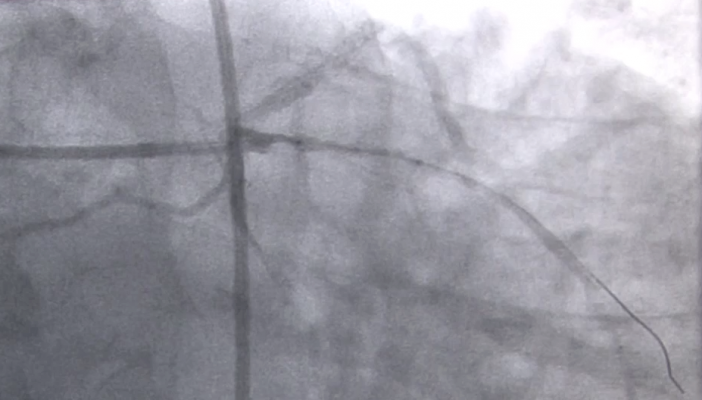
Another possible explanation: Hospital emergency departments are trained to react very quickly when a patient with a suspected STEMI is brought in. For that reason, the time from a STEMI outpatient’s arrival to treatment with angioplasty, referred to as “door to balloon time,” averages about 45 minutes at UNC Hospitals.
"In contrast, when patients who are in the hospital for a non-cardiac condition have a STEMI, the onset is not usually heralded by chest pain and, thus, health care providers may not suspect that a coronary artery has occluded. As a result, the time it takes for restoration of coronary blood flow for inpatients is much slower and more variable," Stouffer said.
These results are based on 48 cases of STEMI among inpatients at UNC Hospitals between Jan. 1, 2007 and July 31, 2011, compared to 227 patients with outpatient STEMI treated at UNC Hospitals during the same time period. UNC Hospitals received the American Heart Association’s Gold Level Performance Achievement Award in 2012 for its care of STEMI patients and has a very active STEMI program. The inpatient STEMI survival rates at hospitals that have not received such AHA recognition may be worse.
For more information: www.ahajournals.org


 January 05, 2026
January 05, 2026 









