January 17, 2012 – Nonstop nosebleeds can be serious and frightening, often sending people to the emergency room, where their noses are packed with gauze. When that doesn’t work, nosebleeds can be halted by injecting microscopic particles – made of the same material as a kitchen sponge – into the arteries that supply the nose. The more blood vessels blocked the better, suggests research being presented at the 24th annual International Symposium on Endovascular Therapy (ISET).
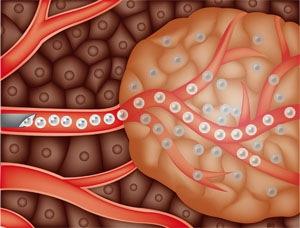
Worldwide, 60 percent of people have suffered nosebleeds, 6 percent of them so severely that they sought medical treatment. These unstoppable nosebleeds are most likely to occur in people who have high blood pressure or are taking blood thinners. Severe anemia from blood loss can lead to complications such as heart attack. Typical nosebleed treatment is to temporarily pack the nose with gauze, inflate a balloon to stop the blood flow or cauterize the blood vessels inside the nose. If those treatments fail, the next options are surgery, or minimally invasive embolization, in which polyvinyl alcohol (PVA) particles are injected into the blood vessels to the nose.
In a study, 84 patients had one to four blood vessels embolized. Nosebleed recurrence rates decreased as more blood vessels were embolized: 2 of 8 (25 percent) who had one blood vessel treated experienced recurrence as did 5 of 35 (14 percent) who had two vessels treated and 2 of 32 (6 percent) who had three vessels treated. None of nine who had four vessels treated experienced a recurrence. Minor pain and complications increased with the numbers of vessels embolized, including mild facial pain, swelling and headache, but were temporary and treated with pain medication.
“Embolization is less invasive than surgery and is very successful, taking the pressure off the fragile lining of the nose and allowing it to heal before the arteries eventually partially reopen,” said Colin P. Derdeyn, M.D., director of the Stroke and Cerebrovascular Center at
Washington University School of Medicine, Barnes Jewish Hospital, St. Louis, Mo. “Our research suggests that the more vessels you embolize, the more successful the treatment.”
To embolize the blood vessels, an interventional radiologist threads a catheter into a groin artery and advances it through the body to one or more of the four arteries that supply the nose, injecting the PVA particles. The particles temporarily stop the blood flow, halting the nosebleed and allowing the area to heal. PVA has been used safely in the body for about 50 years.
For more information: www.iset.org


 January 05, 2026
January 05, 2026 









